Diagnosing velopharyngeal dysfunction (VPD) takes careful listening, testing, data collection and detective work.
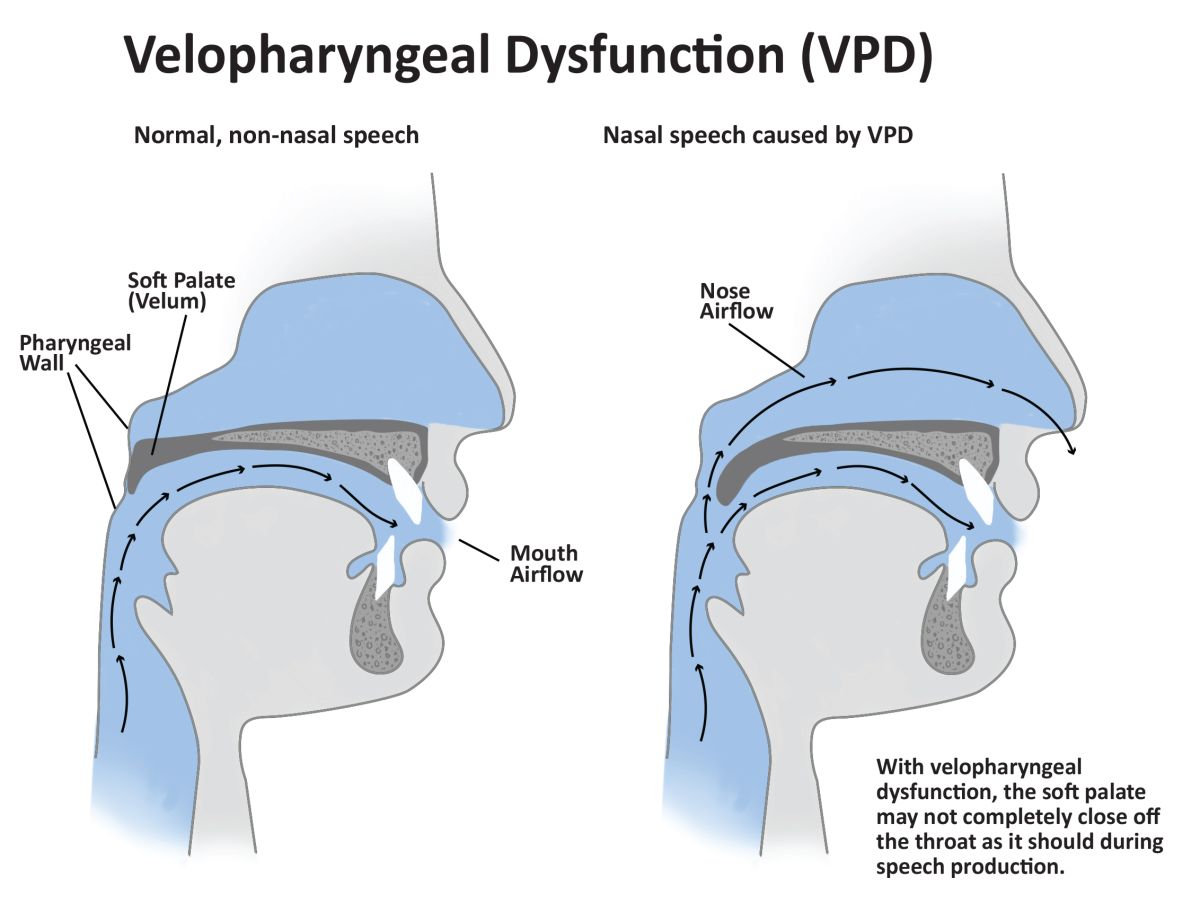
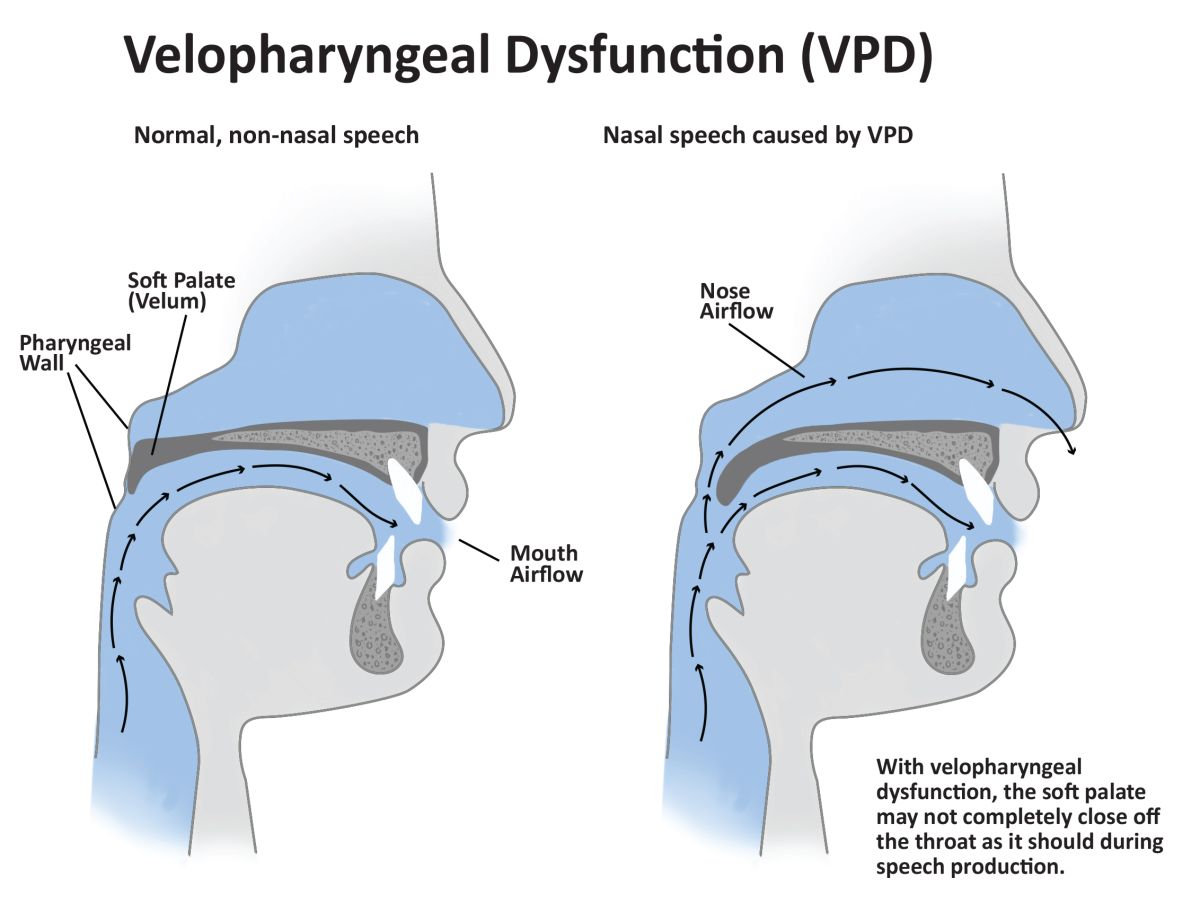
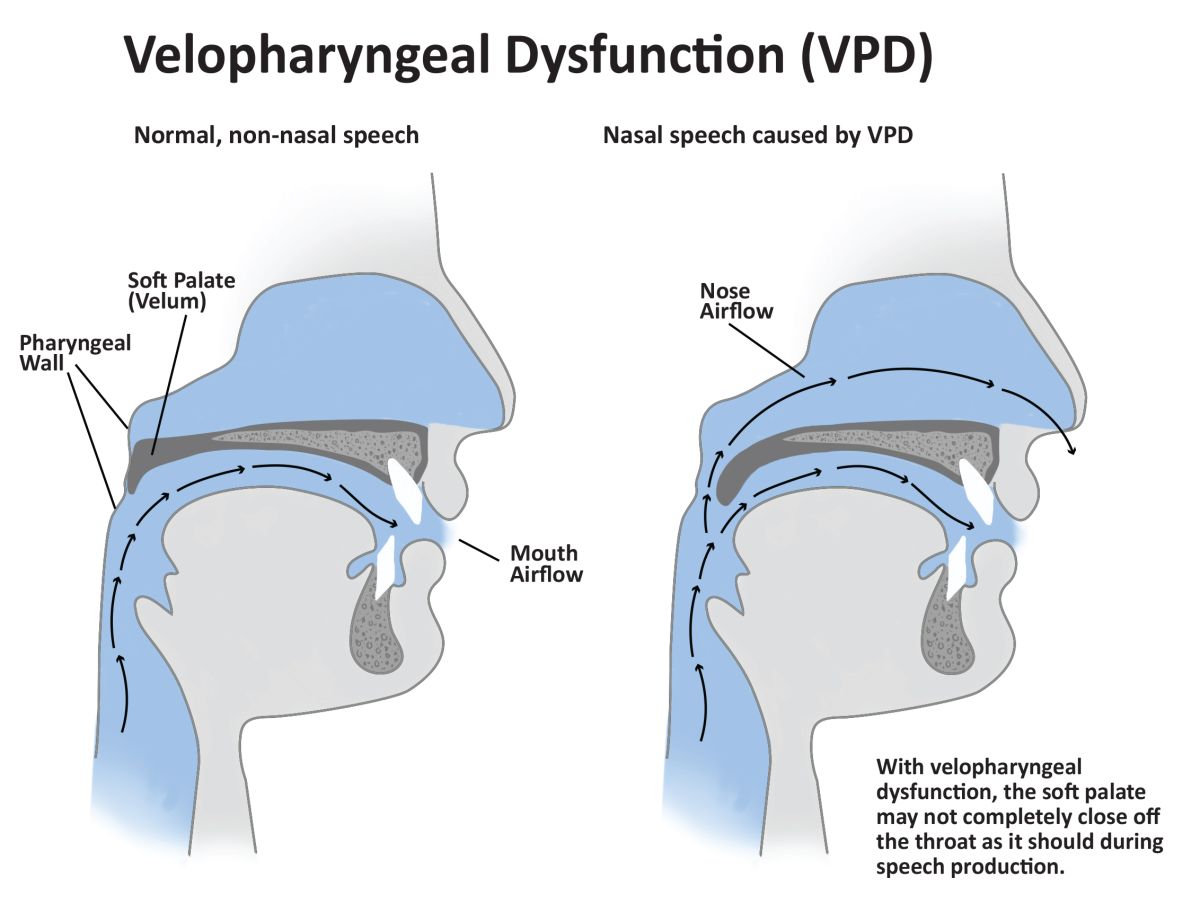
What is velopharyngeal dysfunction? It’s an umbrella term that describes multiple disorders that cause leakage of air into the nasal passages during speech production. Parts of a child’s throat or the roof of their mouth is not working properly and allows air to escape through the nose during speech. Children who are born with a cleft palate are at the most risk for VPD although it can occur in children without a cleft palate. A child’s speech may sound excessively “nasal,” (ie, hypernasal) or on the other end of the spectrum they could sound excessively “congested (ie, hyponasal).”
Gillette Children's speech-language pathologist, Graham Schenck, PhD, has special training in VPD and is an expert in its detection.
Graham Schenck, PhD, is a specially trained speech-language pathologist at Gillette.
The gold standard for diagnosis
“The gold standard for diagnosis of VPD is a comprehensive perceptual speech assessment by a speech -language pathologist trained in assessment and treatment of VPD/resonance disorders,” Schenck says. “It’s a specialty area of our practice where differential diagnosis is quite nuanced. It’s critical to get an accurate diagnosis so you don’t risk recommending surgery for someone who might not need it.”
Many people have never heard of VPD and, according to Schenck, many health care providers think it only occurs in children with cleft palate. “At Gillette we treat many children who have cerebral palsy and have VPD as well. I also see many children with a “hidden” cleft palate called a submucous cleft palate who are referred to us because their speech sounds “nasal” and they’re not progressing well in speech therapy,” Schenck says.
The first step in diagnosing VPD is for a speech-language pathologist to actually hear the difference in a child’s speech. Then the data gathering and detective work begins. “Nasometry is a type of test that uses a handheld, device with a metal plate that acts as a separator. The patient places on the separation plate under the nose. The nasometer measures the ratio of nasal versus oral energy during a simple speech sample,” Schenck says.
If the speech assessment and/or nasometry confirms the possibility of VPD, more tests are ordered such as a nasopharyngoscopy—a small flexible fiberoptic scope that allows a small camera to be inserted into a patient’s nose. The camera allows a speech-language pathologist and surgeon to observe how the soft palate moves while a person is talking. This procedure is done with some medication to help numb the patient’s nose to lessen the feeling of the camera. The patient needs to be awake and be able to talk so their speech and air production can be observed during the nasopharyngoscopy.
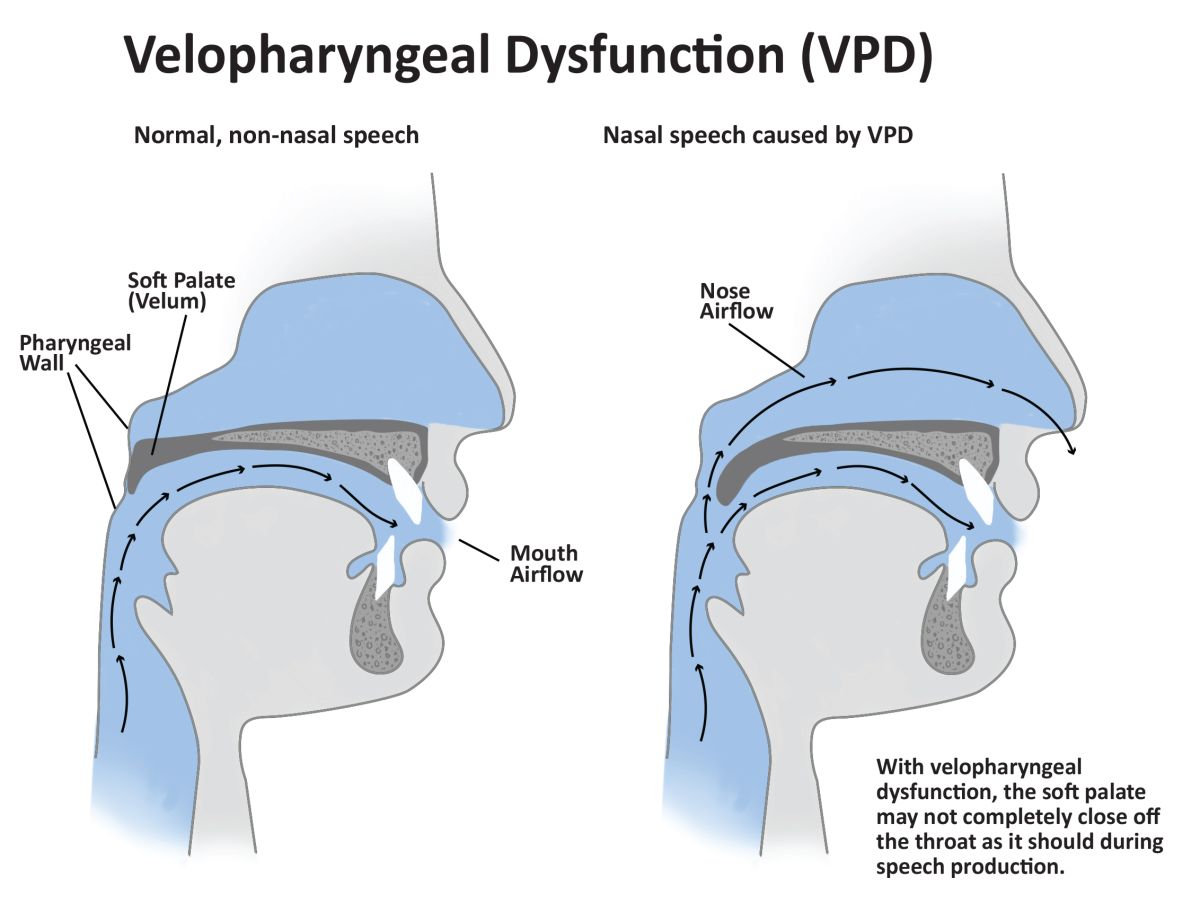
This illustration shows velopharyngeal dysfunction.
A comprehensive and specialty trained craniofacial team
The craniofacial team at Gillette includes speech-language pathologists, craniofacial and pediatric plastic surgeons, neurosurgeons, dentists, orthodontists, advanced practice nurse practitioners, audiologists and other providers who’ve been carefully selected because of their specialized training.
Schenck enjoys being part of a comprehensive and collaborative team at Gillette. “It feels good to be part of an expert team helping children,” Schenck says. He’s also proud of the research being done at Gillette to help refine the diagnosis and treatment of VPD. “We use Magnetic Resonance Imaging (MRI) to assess the muscles of the soft palate in children with various types of cleft palate,” Schenck says. “We’ve had three patients at Gillette enrolled in this research study and the findings will be published soon in a peer reviewed cleft palate journal.”
Schenck says roughly 40 percent of kids with a repaired cleft palate need VPD surgery. He wants to reassure parents that this surgery is needed to restore a normal mechanism for speech. “Kids need the proper tools to be able to speak normally. I often tell parents we would not expect great performance from a car with a leaky gas tank. That’s kind of what VPD is like for kids. The air is leaking out and it’s very difficult, if not impossible, for kids to produce speech normally when that is happening.”
The recovery from VPD surgery is fairly straightforward and short. Children might have a sore throat for a few days and might be on a soft or liquid diet for a while. “Most kids are very resilient,” Schenck marvels. “The VPD surgery is usually less involved than the original repair to the palate.”
Gillette has a comprehensive craniofacial team.
The work we do here changes lives
Schenck enjoys the variety of patients at Gillette. He’s worked with very young children to adults who were not properly diagnosed in childhood. “Some of the most rewarding experiences for me personally come from helping international adoptees and their families.”
One case he vividly recalls involved an older girl who was adopted by parents in Minnesota two years ago. He knew from the first time he saw her that she had VPD and would need surgery and lots of speech therapy to improve her speech.
“Her family was very diligent about her care. She received speech therapy from me and a Gillette colleague and also through her school district,” Schenck recalls. “She had a great surgical repair for her VPD from Dr. Lacey. I saw her recently in clinic and was amazed at her progress and at the quality of her speech compared to when I first evaluated her. It’s now likely she’ll only need another 3 to 6 months of speech therapy and will attain totally normal speech and articulation. Cases like this are why I love what I do at Gillette. The work we do here changes lives.”
Micah and his mom appreciate the expert care from the Gillette craniofacial team.
Meet a care team provider, find a location, learn how to get a second opinion, and more.
Request an appointment to connect with Gillette providers.

