About the Spine
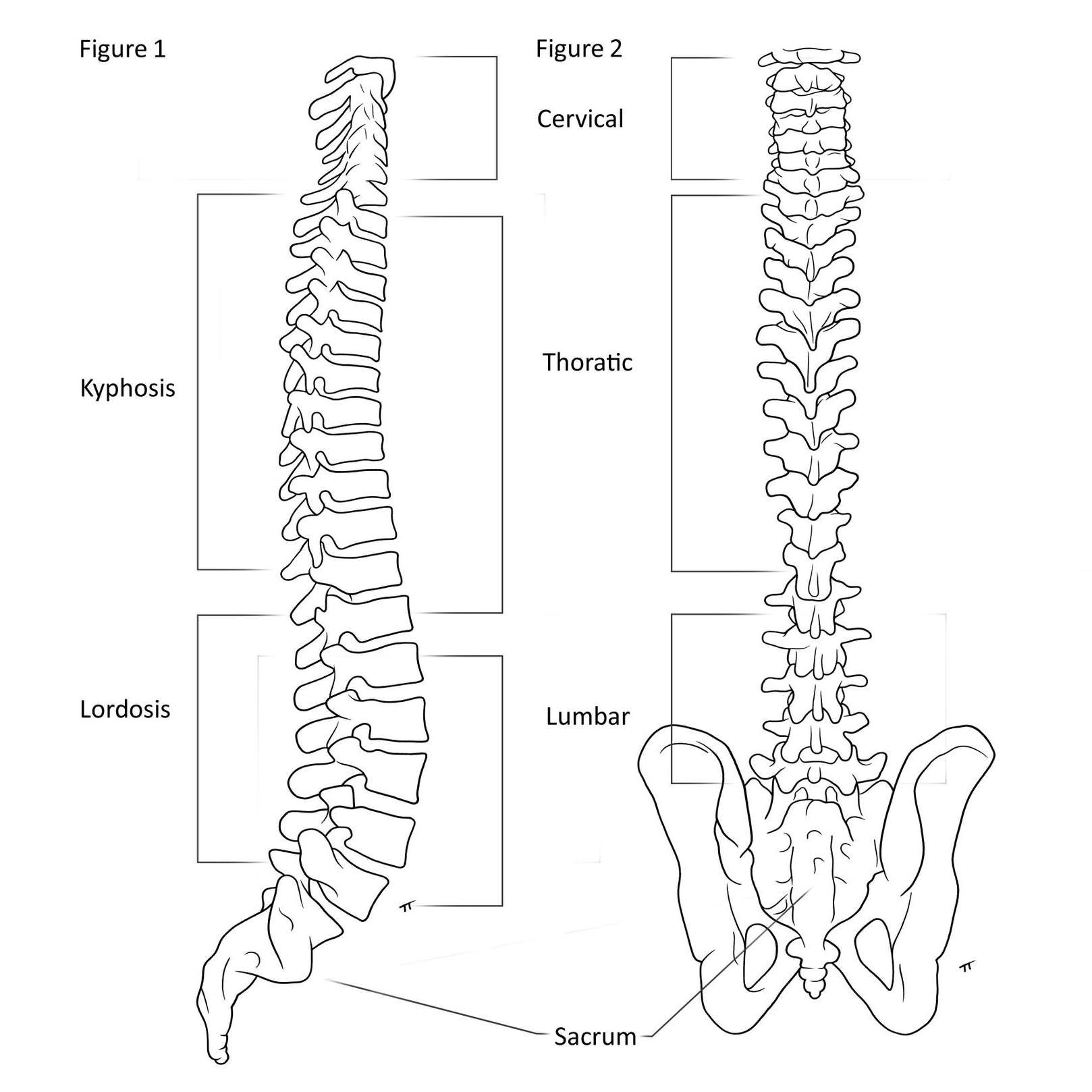
The human spine is made up of 33 bony segments called vertebrae. They fit together, forming a flexible column that supports the back and protects the spinal cord. The neck has 7 cervical vertebrae. The upper back and chest have 12 thoracic vertebrae; these are where the ribs are attached. The low back has 5 lumbar vertebrae. The last lumbar vertebra is attached to the sacrum, which is in turn attached to the pelvis. The lowest part of the spine is the coccyx, or tailbone. When viewed from behind, the spine appears straight and when viewed from the side it has natural curves. There is a natural thoracic kyphosis, forward curving, and a natural lumbar lordosis, backward curving.
What is Scoliosis and Why Do We Treat it?
Some people have extra curves in their back that curve side to side and rotate. This 3-D rotation and side to side curvature is called scoliosis. On an x-ray, the spine of a person with scoliosis looks like an “S” or “C” instead of a straight line. Providers use a special measurement tool to measure the angle of the curve, called a Cobb angle. A slight curve may be normal. Scoliosis is diagnosed when the Cobb angle is 10 degrees or greater.
Idiopathic Scoliosis is categorized based on the age at which it begins:
- Infantile(IIS) less than 3 years old
- Juvenile(JIS) 4-9 years old
- Adolescent(AIS) 10 - 18 years old
Why did I get scoliosis?
The exact reason why your spine curved remains unknown, that’s what “idiopathic” means – that means we don’t know why it occurs. We know there is some basis in genetics. A recent theory involves the front of the spine growing faster than the back of the spine, causing a rotating and twisting of the spine.
You did not do anything to cause your scoliosis. It is not from wearing a heavy backpack; it is not from a “wrong” sleep position; it is not from having poor posture. There was nothing you could have done to prevent getting scoliosis.
Scoliosis is more common than you might think, too. Approximately 3% of people have scoliosis.
Signs, Symptoms and Diagnosis
Most people with scoliosis do not report pain; those that do report pain, typically report only mild pain. Severe or constant pain is not a typical symptom of scoliosis.
You or your parent may have noticed one or more of the following changes in your appearance:
- Chest shifted to one side
- One shoulder blade more noticeable than other
- Asymmetry (unevenness) of the waist
- Clothes fit unevenly
- One shoulder is higher than other
- One hip is higher than other
- Asymmetry of front torso
You may not have noticed any changes in your appearance, but your healthcare provider did when you had your check-up. Your provider may have asked you to do a forward bend exam, which can show spine abnormalities. This is called the Adam’s Forward Bend Test.
The diagnosis of scoliosis is made based upon physical exam, family history of scoliosis, and x-ray of the spine.
Why do we treat scoliosis?
Most patients with mild scoliosis at skeletal maturity (when the spine is no longer growing) will lead a normal life with no limitations on activities, including sports.
However, for patients with more significant curves, there is a higher likelihood that the curve will continue to progress into adulthood. Although it will progress slowly (0.5-1 degree per year), throughout a lifetime this can add up to a significant curve which can be more difficult to correct and have an impact on quality of life.
For significant curves, surgical intervention may be the best option. The decision to have surgery for a curved spine is one that requires discussion with your spine surgeon about your specific curve and how much growing you may have left. It can be a challenge to think about having surgery when you may not be experiencing any discomfort or limitations due to the curve in your spine. But by operating when someone is younger, the curve is smaller and more flexible. That means we can operate on the smallest section of the spine, preserve as much motion in the spine as possible, and have quick and effective healing.
Scoliosis Surgery Explained
When spinal curves progress to a more significant degree, surgery may be the best option. For those who may benefit from surgery, the two options are spinal fusion and vertebral body tethering.
Fusion Spine Surgery
Spine fusion involves joining two or more individual bones to make one unit.
Posterior Fusions
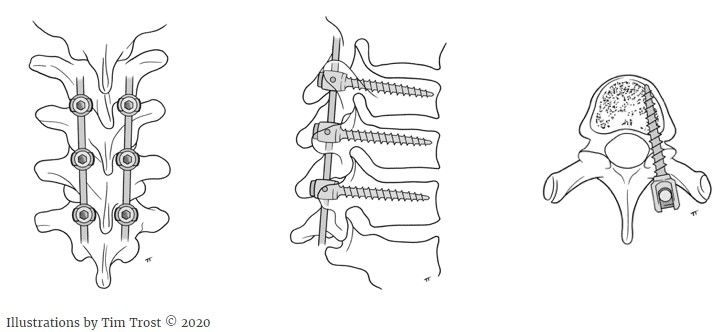
These are the most common scoliosis surgeries. Spine surgeons correct most curves by going through a patient’s back. They then attach screws or anchors to the individual bones of the curve, connect the anchors with smooth rods, and then move the spine into a more straight position.
Anterior Fusions
Spine surgeons can stop some curves from progressing by fusing the front of the spine. A spine surgeon works with a general surgeon to open the chest or abdomen through the side. The surgeon may insert screws and a smooth rod to hold the spine in place while fusion occurs.
Vertebral Body Tethering
Recent advances in the treatment of AIS include strategies that harness the body’s growth to correct the spine deformity without the need for spinal fusion. In this surgery, a spine and a general surgeon work together to go through the chest or abdomen, placing screws in the vertebral bodies on the convexity (outside) part of the curve and connecting the screws with a strong rope (tether). The tether is tensioned to slow down growth on the curve convexity while allowing for continued growth on the concave (inside) part of the curve. As such, the body’s natural growth allows for curve correction with time. Because the success of the procedure relies on spine growth after the procedure, patients need to meet very specific criteria to be a candidate for this surgery.
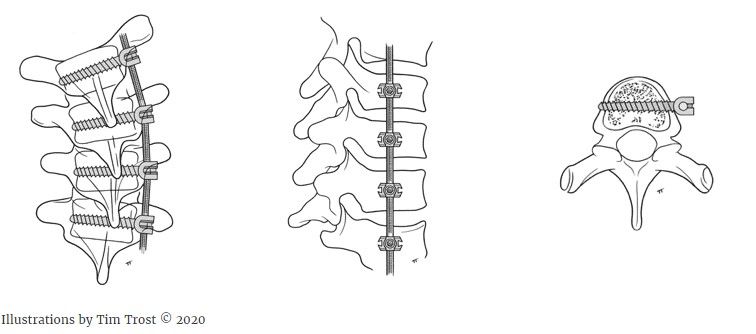
For patients with early onset scoliosis with larger spine curves, magnetically controlled growing rods may be needed to help control the curve while the child continues to grow.
Magnetically Controlled Growing Rods
Magnetically controlled growing rods can be surgically inserted on the spine. These rods have the ability to be lengthened a small amount during a routine clinic visit through the utilization of an external remote control every three to six months. The goal with magnetically controlled growing rods is to allow a child’s spine to continue growing while minimizing the need for multiple repeat surgeries and preventing rapid progression of the curve.
Scoliosis Stories as Told by Our Patients
Olivia had scoliosis surgery when she was 18. This is her story.
Ellie had scoliosis surgery when she was 14. This is her story.
Mattie had scoliosis surgery when she was 13. This is her story.
Planning for Surgery
Preparation for surgery
Your surgeon will meet with you before surgery to go over risks and benefits, discuss the specific levels of your surgery, and answer any specific questions you might have.
Exercise
Before surgery, take part in regular physical activity, such as walking. Physical exercise tends to improve bowel function and helps you stay as healthy as possible. Additionally, if you’re physically active before surgery, you’ll find it easier to regain your abilities afterward.
Diet
Protein is very important for healing. We suggest increasing your consumption of protein six weeks before surgery. If you’re concerned about weight gain, trade servings of protein for servings of carbohydrates. This diet should be continued following surgery as well. See page 00 for more information.
Pre-op History and Physical
Within 30 days of your surgery, you must see your primary care provider for a pre-operative (pre-op) History and Physical. This is to make sure you are healthy enough to undergo surgery. You will also have blood taken to check your hemoglobin. This measures how much oxygen your blood can carry, and will be a measurement we will also check after surgery. This is required of all patients undergoing surgery at Gillette.
Tour Gillette
We offer (and encourage!) our patients and their families to take a tour of Gillette before surgery. This is not only a tour of the building; our child life team will discuss various coping mechanisms and resources available to make your stay as comfortable as possible. They will also assess what the patient and family may be most anxious about regarding their surgery and hospital stay, and use various techniques to lessen this anxiety as much as possible. We recommend this visit within 2-3 weeks before surgery.
Medications
Please do not take any NSAID medication within 1 week of your surgery (ibuprofen, Motrin, Aleve, naproxen). These medications alter the way the blood clots and can increase the risk of bleeding during surgery. Tylenol is okay to take.
Day Before Surgery
You will receive a pre-op shower kit from Gillette. This has a special anti-bacterial body wash and shampoo. The night before surgery, you must wash your entire body and hair with this soap. Then, sleep on clean sheets wearing clean pajamas. The morning of surgery, you must shower again and wash your entire body and hair with this soap a second time. This is one of the many steps we take to decrease your risk of infection.
Day of surgery
Check-In
You will be instructed to arrive 1.5 hours before your scheduled surgery time. Please take the elevator to the 3rd floor and check-in at the desk.
Pre-Op Area
When you are called back, you and your caregiver will be led to your room inside the pre-operative area. You will change into a gown and special warming wrap. You will meet the pre-op nurses who will ask questions and measure your pulse, oxygen level, blood pressure and temperature. These measurements are known as your “vitals.” After that, you’ll discuss with the nurses if one caregiver will go with you to the operating room (OR) while you fall asleep for surgery. This caregiver must wear a special cloth covering (“bunny suit”) over their clothes to keep the OR clean and free from germs. They will “suit up” in your pre-op room.
Meet Your Care Team
Before surgery, you will meet the care team who will work to keep you safe and comfortable before, during, and after your surgery.
Your pre-op nurse is a registered nurse (RN) who will help you get ready for surgery once you arrive at the hospital.
Your anesthesiologist is the doctor who will help you fall asleep for surgery, make sure you are safe, breathing well, and kept warm during surgery. They will also help manage your pain after surgery with IV pain medication. In the pre-op area, the anesthesiologist will develop a plan with you and your family for keeping you comfortable with different medication options.
Your nurse anesthetist works directly with the anesthesiologist and is with you at all times during surgery to make sure you are safe, breathing well, and kept warm during surgery.
Your surgeon will see you before your surgery to answer any questions you may have. They will also use a purple marker to mark the area you will be having surgery to make sure that everyone agrees on what part of the body will be operated on.
The operating room (OR) nurse is the RN who will be with you during your surgery. They help the surgery team and will be calling your caregiver with updates throughout the procedure.
During surgery
After you drift off to sleep, a tube will be inserted into your windpipe to help you breathe during surgery. Then the team will continue to prepare you for surgery by inserting a catheter into your bladder, inserting more IVs, and placing multiple stickers and small needles (similar in size to acupuncture needles) into muscle groups throughout your body. These stickers and small needles allow us to monitor your spinal cord during surgery. After that, we will position you for surgery, clean your skin again and begin the procedure.
Your caregivers must stay in the Regions building during your surgery so the OR nurse can call them with updates as your surgery progresses.
**Caregivers, please keep your phone alerts turned on so you can hear it ring when the nurse calls to update you. The OR nurse will call you every 1-1.5 hours with updates on the procedure. **
Recovery After Surgery
After surgery
After surgery, the medications that keep you asleep will be turned off and the breathing tube will be removed. You will then be taken to the post-anesthesia care unit (PACU) to continue waking up and start receiving pain medication. Your nurse will invite a caregiver to join you when you are ready. Hospital policy limits the number of visitors allowed in the PACU, but once you move to the orthopedic surgical unit (OSU), all of your visitors can see you.
When you are ready to leave the PACU, you will be taken to the orthopedic surgical unit. This is where you will spend the rest of your recovery in the hospital. You will have a private room with a couch that turns into a bed for one of your caregivers to stay the night. Hospital policy states that no visitor under the age of 18 years old is allowed to spend the night at the hospital.
After surgery, your body is at risk of certain complications. We’ll do many things to reduce those risks. A nurse will be checking on you frequently (every 1-2 hours) to help you reposition and give you medications. Your nurse will also check your vitals and check your arms and legs for color, movement, sensation (sense of touch), circulation (blood flow) and pulse.
Medical Equipment
As you recover from surgery, you might need some or all of the equipment pictured here. Each piece plays a role in helping you heal.

An incentive spirometer is a breathing aid. Used with deep breathing and coughing exercises, it helps keep your lungs healthy after surgery.
A patient-controlled analgesia (PCA) pump is a machine that delivers pain medicine during the first day of your recovery.
An intravenous (IV) pump delivers the fluids that your body needs after surgery. We attach a bag of IV fluid to a tube that’s inserted into a vein in your hand, arm or foot.
A vital-signs monitor is a machine that keeps track of your heart rate and breathing status. We attach the monitor to your chest with small sticky patches and tape a wire to your finger or toe. A red light on your finger tells you that the monitor is working.
Oxygen, used after surgery, makes it easier for you to breathe. Sometimes an oxygen mask covers your nose and mouth or is placed next to your face. In other cases, a small tube (called a nasal cannula) rests under your nose.
A sequential compressing device (SCD) increases circulation in the legs and helps prevent blood clots. You’ll wear soft leg or foot wraps. The machine pumps air into air pockets in the wraps, then releases it.
Braces (orthoses) support and protect your back. You might need to wear one after surgery.
A surgical drain (Hemovac) is a tube that runs from your incision to a plastic container. It collects fluids and blood from around the incision and it’s removed when drainage decreases. This will be removed while you are in the hospital before you go home.
A small chest tube is inserted into the space between your lungs and ribs. It helps to keep your lungs healthy and inflated after surgery. This will be removed while you are in the hospital before you go home.
A Foley catheter is a small tube, inserted into your bladder that drains urine after surgery. Your nurse will check it often.
Surgical Dressing
Your nurse will check your surgical dressing (a large band-aid that covers your incision) regularly. We will remove it after you shower on the second or third day after surgery. You’ll notice small strips of tape called Steri-Strips, or one long piece of tape called Prineo tape, which hold your incision together. We will put a new dressing over your incision and keep it covered while you are in the hospital. The Steri-Strips or Prineo tape will fall off about one to two weeks after it is applied; you should not pull it off, let it fall off on its own. The stitches in your back are under your skin and will dissolve on their own after about three weeks. You do not need to have any stitches removed.
Managing Pain
Pain is to be expected and is a normal part of healing after surgery. Pain is different for everyone, but patients often report the first three days at home as being the most challenging; then things get much better. You can expect ups and downs with pain relief. It’s common to have times when pain increases—especially when activity increases, too.
Resuming a regular diet
After surgery, your care team will listen for bowel sounds through a stethoscope placed on your stomach. You won’t be allowed to eat or drink anything until you have bowel sounds. Bowel sounds tell us that your digestive system has “woken up” and will be able to process food. If you start to eat too soon after surgery, you can feel nauseous. After you have bowel sounds, you may begin taking ice chips or small sips of water. We’ll gradually add to your diet as you’re able to tolerate food. During surgery and before you resume eating, your IV will provide the fluids your body needs. As your recovery progresses, you’ll begin eating solid foods. Once you’re taking fluids, solid foods and pain medicines by mouth, we can take out your IVs.
It is common to have less appetite for a few weeks after surgery. The pain medicine can decrease your appetite. Also, you are not being as active, so the body does not need as much food for energy. It is important to try and eat balanced, small meals, or healthy snacks throughout the day. Food is very important to help your body heal well and quickly.
A good diet helps minimize issues — such as constipation and other intestinal problems — that are sometimes associated with surgery. For example, regularly eating a high-fiber diet is helpful. To avoid gas and bloating, increase the amount of fiber in your diet gradually.
The following foods are good sources of dietary fiber:
Cereals: Bran cereals, grits and oatmeal as well as processed cereals like Cheerios, Chex, Cracklin’ Oat Bran, Fiber One, Grape-Nuts and Wheaties
Breads: Bran muffins and whole-wheat, cracked-wheat, rye or multi-grain breads
Grains: Barley, brown rice, buck wheat, bulgur, cracked wheat, rolled oats, whole-wheat pasta and wild rice
Legumes: Black beans, chickpeas (garbanzo beans), kidney beans, lentils, navy beans, pinto beans and white beans
Nuts and Seeds: Almonds, Brazil nuts, coconut, hazelnuts, peanuts, peanut butter, popcorn, pumpkin seeds, sesame seeds, sunflower seeds and walnuts
Fresh or dried fruit: Apples, apricots, avocados, berries, cherries, dates, grapefruit, grapes, kiwi, mangoes, melon, nectarines, oranges, papayas, peaches, pears, pineapple, plums, raisins, rhubarb and tomatoes
Vegetables: Asparagus, beets, broccoli, cabbage, carrots, celery, corn, eggplant, green beans, lettuce and leafy greens, onion, parsnips, peas, potatoes, spinach, sweet potatoes and zucchini
Hydration
Drinking plenty of fluids causes the intestine to contract, moving stool through the large intestine. Water and fruit juices are especially beneficial. Be sure to drink six to eight glasses of water a day. Water is the best option. If water is not your favorite, try adding a water flavoring. Fruit juices don’t have fiber, but they — especially prune juice — have components that can help manage constipation. Peach, pear, papaya and citrus juices are good choices, but limit yourself to 4 to 8 ounces of fruit juice each day. To avoid constipation, limit milk and dairy products to 3 to 4 servings each day.
If you’re drinking more than one or two cans (20 ounces total) of soda, or more than one or two cups of coffee per day, try to cut back. High amounts of caffeine intake can delay healing as well. Be aware of your caffeine intake before and after surgery and use it in moderation.
Personal grooming
- If your sink is lower than your waist, kneel on the floor or a low footstool in front of the sink.
- If your sink is waist level or higher, support your upper body with a bent forearm. Place one leg slightly behind you.
- Wash your hair while standing or sitting in a shower.
- Use a bath mat or slip-resistant strips on the shower floor. Make sure the floor is dry before you step onto it.
- If you must wash your hair at a sink, use a spray nozzle to avoid bending forward.
- To avoid twisting and bending, use soap-on-a-rope, a long-handled scrub brush, or a hand-held shower nozzle to extend your reach.
- The most difficult areas to wash, without bending forward, are your legs and feet. When washing your legs and feet, or putting on socks and shoes, use a footstool. Or cross one foot over the opposite knee.
- When sitting on a toilet, keep your back tall. Avoid twisting as you wipe.
Dressing
- While you’re recovering from surgery, avoid using bottom drawers or closet floors to store your clothes.
- Before dressing, gather the clothes you plan to wear (including socks and shoes), so you don’t have to make multiple trips to your closets and drawers.
- Select comfortable, loose-fitting clothes and slip-on shoes.
- Wear button-front shirts, or put your arms through the sleeves of pullovers before you draw them over your head. As much as possible, avoid twisting and bending.
- For girls, sports bras can be challenging to put on because they require you to lift and move your arms and shoulders. Our patients have found that front-clasp or back-clasp bras are most comfortable and easiest to take on and off.
- Sit on the edge of a bed or chair to dress.
Driving
- You should not drive if you are taking narcotics or Valium for pain.
- If you drive, you may resume doing so as soon as you’re comfortable and certain that you can react quickly by braking or swerving. Practice driving in a long, quiet driveway or an empty lot at first.
- On long trips—whether you’re the driver or the passenger—stop every one to two hours and walk around for 5 to 10 minutes.
Caring for incisions and minimizing scars
After you have been home for 24 hours, you may remove your dressing on your incision. There will be Steri-strips or Prineo mesh tape over your incision. This should be left in place and allowed to fall off on its own, do not pull it off. If edges begin to roll up and are bothersome, the loose edges may be trimmed with scissors. You do not need to put a new dressing or bandage on.
Avoid submerging yourself in bathtubs, pools, hot tubs, whirlpools or lakes until your doctor says it’s OK to do so (at least 6 weeks after surgery, when your incision has healed). If water seeps into your incision, it could cause an infection. You may, however, let soapy water run over your back. You should shower, or use a wet cloth, to wash your body at least once every two days. Gently pat your incision dry, using a clean towel. Avoid rubbing or scrubbing your wound. It is safe to wash your hair.
Watching for Infections
Check the surgical incision daily for signs of infection. A healing incision might look pink, but it shouldn’t be inflamed or deep red. Symptoms of an infection may include:
- Warmth, redness, draining or swelling at the incision site
- An ongoing fever of 100.5° Fahrenheit, 38° Celsius or higher
- Pain
- Numbness, tingling or weakness in your legs (numbness of the skin around the incision is normal)
Minimizing Scars
Do not use any lotions or creams on your incision unless approved by your provider. Typically, scars remain raised, red and firm for eight weeks. After a year, they usually become softer, paler and flatter.
To reduce scarring, shield your incision from sun exposure for a full year.
Bowel Management
Constipation is very common after surgery and can be a significant source of discomfort. The anesthesia, pain medications, and lack of activity all contribute to the gut moving slower which results in constipation. There are many methods to manage constipation. Keep in mind that bowel management is different for everyone.
The goals of bowel management include:
- Emptying the lower bowel at regular intervals
- Preventing constipation
- Preventing pain and discomfort
- Promoting independence
While you are in the hospital you will begin taking two medications by mouth, Senna and Miralax, to help promote gut movement and soft stool. In the hospital, you may require a suppository or an enema to help promote bowel emptying. These medications are inserted into the rectum. Coffee and caffeine can also help promote bowel movement, but high amounts of caffeine intake can delay healing. Be aware of your caffeine intake before and after surgery and use it in moderation.
Once you are home you will continue to take the oral these medications every day while you are still taking narcotic pain medication. If you go 48 hours without having a bowel movement, it is recommended that you use a suppository to help promote bowel emptying. If that is unsuccessful, it is recommended that you use an enema. Both suppositories and enemas can be purchased over the counter at any pharmacy, Target, or Walmart. If at any time you are having significant abdominal bloating, discomfort or are vomiting when trying to eat, please call our 24-hour Telehealth Nurse Line for assistance. If you develop loose or watery stools, stop taking the Senna and Miralax until the loose stools subside.
It’s easier to have a bowel movement when you’re sitting, rather than lying down. If your feet don’t touch the floor when you sit on a toilet, put a box or footstool under them so that your knees are higher than your hips. This squatting position helps promote bowel emptying.
Constipation
For Parents
Mobilizing and repositioning
Once home, you will spend the majority of your time resting. Repositioning frequently (about every 2 hours) reduces your risk of pressure wounds forming on the skin. We will practice repositioning with you and your caregivers while you are in the hospital.
It is also very important that you continue to walk multiple times throughout the day. The recommendation is to walk a short distance, such as to the kitchen or bathroom, at least once every 2 hours during the day. This will keep your muscles strong, prevent stiffness, and promote healthy lungs after surgery. See How to Move Safely after Surgery (Appendix 2).
**For Caregivers**
You will play an important role in helping to reposition, mobilize, and motivate your child to move after surgery. Being involved and asking questions while you are in the hospital will help you to feel more comfortable with these tasks once you’re home. Your child will likely need frequent repositioning, help with toileting, hygiene, and medication management.
Prepare to bring your child home after surgery
Spine surgery is a significant event in your and your child’s life. It can be difficult to see your child in pain during the recovery process. The information in this manual explains how you can help ease their pain. Of course, we are always available to answer any questions or concerns you have.
After surgery, the first few days at home may be challenging. Many parents compare it to having a newborn at home. Your child will likely need assistance with many daily activities including using the bathroom, dressing, personal hygiene and getting around the house. You will also be responsible for their pain medications. It is important to reposition your child frequently, about every 2 hours, to prevent pressure wounds and skin breakdown. Many patients become uncomfortable when lying in one position and may ask you to help them reposition more frequently. Pillows, blankets, or towels rolled into a log shape can help to reposition your child at home.
The frequent needs of your recovering child can be a lot to take on. Having support from family and friends to help care for your child and give you rest is important. Plan to have a few family members or friends scheduled to stay with your child so you can take a break in the first couple of weeks at home or ask for meals that are easily stored and cooked.
If you need the Family Medical Leave Act (FMLA) paperwork filled out for your employer, please inform your surgical team before surgery. This ensures your employer has the necessary information about your absence to help your child recover.
Home Recovery Preparation
- Sleeping: If your child’s bedroom is up or down any stairs, consider having them sleep on the main floor for the first few nights at home. Stairs are safe after surgery but can be uncomfortable for the first few days.
- Showering: Standing for prolonged periods in the shower can be uncomfortable. Place a chair or stool in the shower your child can sit on. A lawn chair or folding chair with a towel on it will be waterproof and safe from slipping.
- Cook meals that can be frozen or reheated easily.
- Have a notebook to keep track of pain medication timing and dosing. Some families set an alarm on their phone as a reminder to take medications at the correct time.
The Trip Home
About an hour before leaving the hospital, our nurses will recommend you take a full dose of pain-relief medicine. If you have a long drive and pain relief is needed, take medicine as prescribed during the trip. You also might want to stop often. Repositioning promotes good circulation and comfort. Be sure to wear a seat belt!
Pain at Night
You might notice more pain at night. When we lay down to sleep at night, our brains are no longer distracted by the world around us and can begin to focus more on any discomfort we are feeling. Using calming techniques –breathing, meditation, etc., in addition to pain medications can help with pain at night. See Relaxation Techniques (Appendix 3), for more ways to relax muscles and provide comfort.
Pain-Relief Medicine
We use multiple pain-relief medications to help manage pain after surgery. While it may seem like a lot of medication, we have multiple options to help manage different types of pain. The medications are safe to be taken as prescribed, including if you are instructed to take two medications together.
Be Careful With Medicines!
Do not use nonsteroidal anti-inflammatory (NSAID) medications if you’ve had a spinal fusion. These medicines can affect bone healing. They include ibuprofen (Motrin and Advil) and naproxen (Aleve). Please avoid these for 3 months after surgery, unless specifically told otherwise by your provider.
Because many over-the-counter medicines contain acetaminophen, always read labels to keep from using too much.
Other Pain-Relief Methods
Music, stories, books, television, video games and other activities can help distract you from pain. Massage or a soothing touch—especially on areas of the body that are pain-free—can help as well. See Relaxation Techniques (Appendix 3), for more ways to relax muscles and provide comfort.
If Pain Increases
Swelling, activity, anxiety, infection and poor sleep can increase pain. If pain is worse than usual, take another dose of pain-relief medicine if enough time has passed since the previous dose. If you aren’t already using it, try stronger pain-relief medicine, such as narcotics prescribed by your health care provider. Never take more medicine than your doctor prescribes!
You might have pain in your legs, back, chest or ribs as you recover. Spine surgery is a significant change for your body. When we move the bones of the spine, we also move the parts of the body connected to the spine including shoulder muscles and bones, stomach muscles, etc. If pain worsens, first review your daily activities. Discomfort often is your body’s way of telling you that you need to rest. Increase activities gradually. Anticipate increases in activity and take pain-relief medicine an hour before exercising, standing or walking. It’s better to use pain-relief medicine and be active than to limit activities to avoid pain.
Check on bowel habits. Constipation can contribute to pain and can be felt as pain in the back. See below for tips on preventing and managing constipation.
When to Call Telehealth for Pain Concerns
If any of the following symptoms are occurring after using pain medications as prescribed, trying the pain relief strategies outlined above, and having a recent bowel movement, please call Telehealth for further evaluation and guidance:
- Difficulty breathing or unable to hold a conversation
- Change in mobility (for example: was able to walk a short distance, but is no longer able to because of pain)
- An ongoing fever of 100.5° Fahrenheit, 38° Celsius or higher.
Discontinuing Pain-Relief Medicine
After being home for 2 to 3 days, you should begin to gradually wean off of the strong narcotic pain medication. By day 7 at home, you should no longer need Oxycodone, Valium or Vistaril. You should continue to take Celecoxib and Tylenol as prescribed. Before going home, nursing or pharmacy will review a specific plan for you to discontinue pain-relief medicines. See your medication list.
**For Caregivers**
At Gillette, we know narcotic pain medications can cause addiction. We follow the guidelines set by the State of Minnesota and prescribe the lowest amount of medication necessary to help recovery from a procedure. If you are concerned about your child or anyone in your life having access to pain medication or are concerned about addiction potential, please discuss these worries with your surgeon as soon as possible.
Scoliosis Stories as Told by Our Parents
Taya's Story
Jill's Story
Additional Resources
Additional Resources and Support
-
What is Scoliosis?
Scoliosis is a sideways curve of the spine. This is a common condition that can leave the spine looking like an “S” or a “C,” rather than a straight line down the back.
National Scoliosis Foundation
Find more information about scoliosis, including answers to common questions, a glossary of terms related to scoliosis and links to additional resources.
Scoliosis Resource Group on Facebook
This Scoliosis Resource Group provides support and information to people who have scoliosis and to their families. All members of the community can come together to pose questions, celebrate achievements, share advice and provide support to one another.
Research at Gillette
Gillette is committed to providing the best, safest, and most up to date treatment options for scoliosis. As an organization, we participate in research to continue to learn and develop our techniques and share these with the scientific and patient community.
Patients who agree to help us conduct this research are a very important part of this process. You may be asked to participate in a research study during your surgery process.
This information is for educational purposes only. It is not intended to replace the advice of your health care providers. If you have any questions, talk with your doctor or others on your health care team. If you are a Gillette patient with urgent questions or concerns, please contact Telehealth Nursing at 651-229-3890.


