What is a spinal cord injury?
A spinal cord injury disrupts the normal communication that flows between the brain, the spinal cord (the thick cord of nerve tissue located within the bones of the spine), and the peripheral nerves. This disruption can lead to loss of movement (paralysis) and loss of sensation—including the ability to feel heat, cold and touch—below the area where the spinal cord is injured. Spinal cord injuries can be caused by trauma, infection or disease.
What are the effects of a spinal cord injury?
Spinal cord injuries affect people differently. The location and severity of the spinal cord injury usually determines the kinds of effects the injury will have.
The location of the injury on the spinal cord matters. Injuries higher up on the spinal cord affect more areas of the body than those lower on the back do.
For example, a neck-level injury could cause paralysis in both arms and legs (also known as quadriplegia) and make breathing without a ventilator impossible. An injury lower on the spinal cord might affect only the legs (known as paraplegia) and lower parts of the body.
The spine is made up of 33 small bones called vertebrae. The vertebrae are grouped into four categories based on their location on the spine.
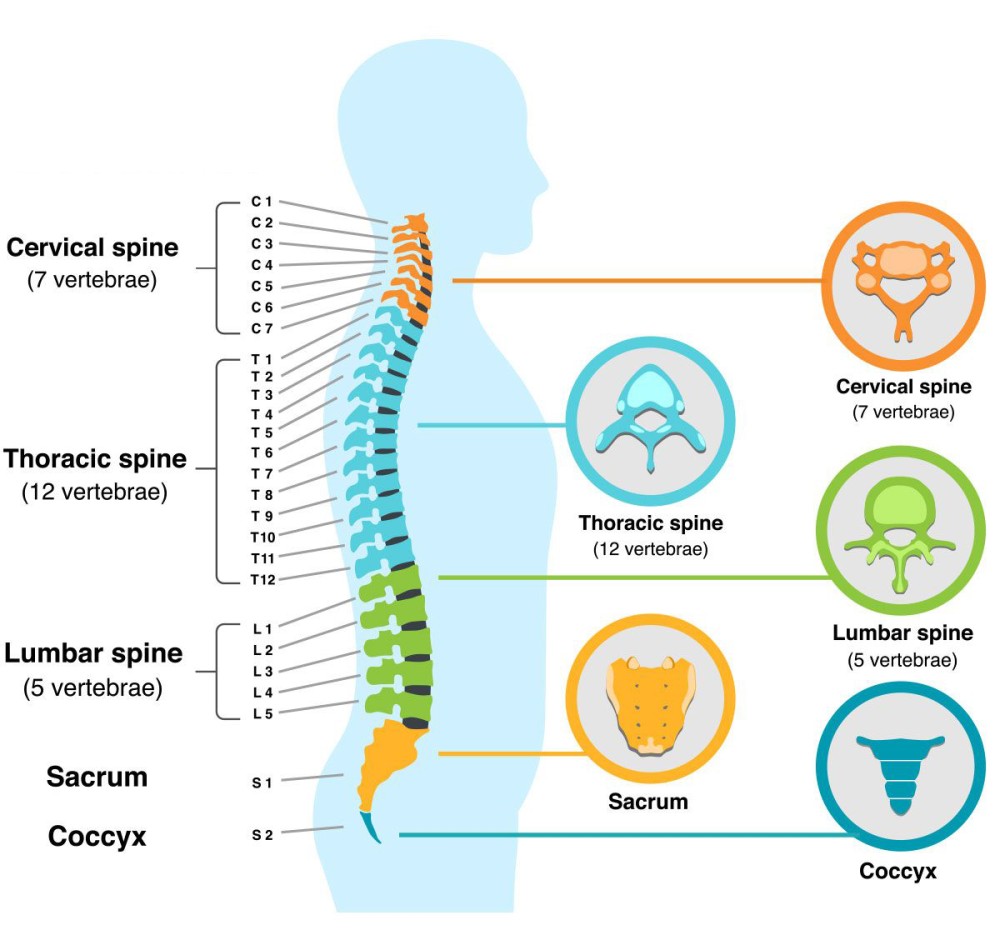
Human Vertebral Column
- Cervical spine (vertebrae C1 through C8): The uppermost part of the spine, where the neck is located. C1 is the vertebra closest to the skull.
- Thoracic spine (vertebrae T1 through T12): The second highest part of the spine, spanning the upper and middle back. T1 is closest to the neck.
- Lumbar spine (vertebrae L1 through L5): The lower back area. L1 is highest on the spine.
- Sacral spine (vertebrae S1 through S5): Between the lower back and the tailbone. S1 is highest on the spine.
Health care providers often refer to the specific vertebra associated with the different spinal cord injury levels. Physical therapists and occupational therapists at Gillette also use these levels to create a rehabilitation plan after injury. Click through the module below to learn more about the different symptoms associated with spinal cord injuries. At Gillette, we address these symptoms with specific physical therapy and occupational therapy for each spinal cord injury level.
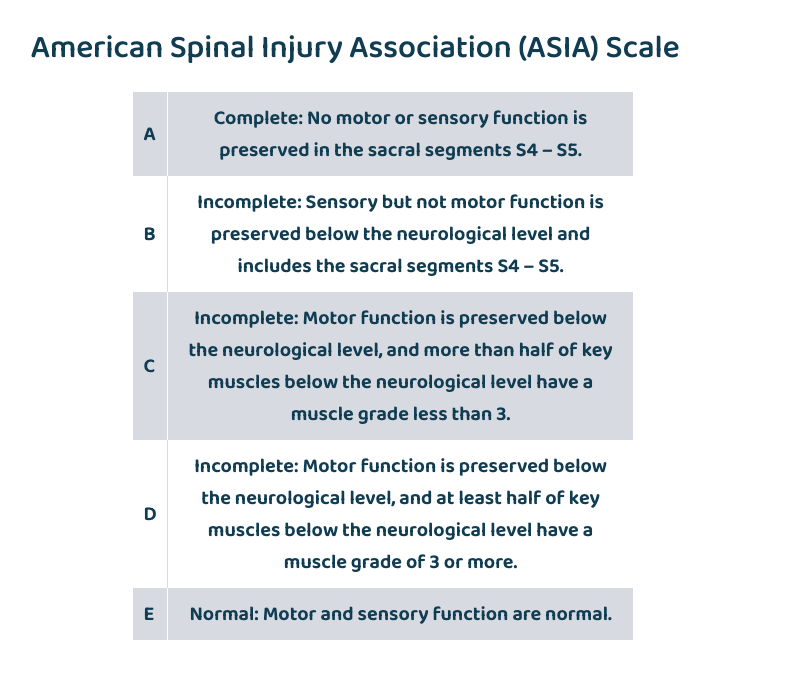
Spinal cord injuries range in severity. With an incomplete injury, the spinal cord can communicate some messages to and from the brain. Children who experience incomplete injuries might retain some sensation and motor function below the injury. With a complete injury, however, all motor function and sensation below the injury is lost.
Gillette Children’s uses the American Spinal Injury Association (ASIA) Scale to describe how severe an injury is.
American Spinal Injury Association (ASIA) Scale
| A | Complete: No motor or sensory function is preserved in the sacral segments S4 – S5. |
|---|---|
| B | Incomplete: Sensory but not motor function is preserved below the neurological level and includes the sacral segments S4 – S5. |
| C | Incomplete: Motor function is preserved below the neurological level, and more than half of key muscles below the neurological level have a muscle grade less than 3. |
| D | Incomplete: Motor function is preserved below the neurological level, and at least half of key muscles below the neurological level have a muscle grade of 3 or more. |
| E | Normal: Motor and sensory function are normal. |
Spinal Cord Injury Video
Watch the video below to learn more about the different symptoms associated with spinal cord injuries. At Gillette Children's, we address these symptoms with specific physical, occupational, and speech therapies as well as comprehensive inpatient physical rehabilitation as needed.
Sliding Down the Spine: What Kids Should Know About Spine Injuries
 Home Page
Home Page

