Single-Event Multi-Level Surgery, or SEMLS, is a series of procedures performed during one surgery in order to correct soft tissue and bone problems that are often associated with an underlying neurological or orthopedic condition. SEMLS is a common part of treatment plans for individuals with cerebral palsy and spina bifida, among others.
This page describes the surgeries that Gillette surgeons perform on the lower body (legs and feet, or “lower extremities”). Some surgeries will look slightly different than what is shown here, depending on your age and your doctor.
SEMLS Bony Procedures
Some surgeries cut into your bones to help improve alignment of your legs and feet. Proper alignment enables you to be in the right position to strengthen your muscles and improve your ability to walk.
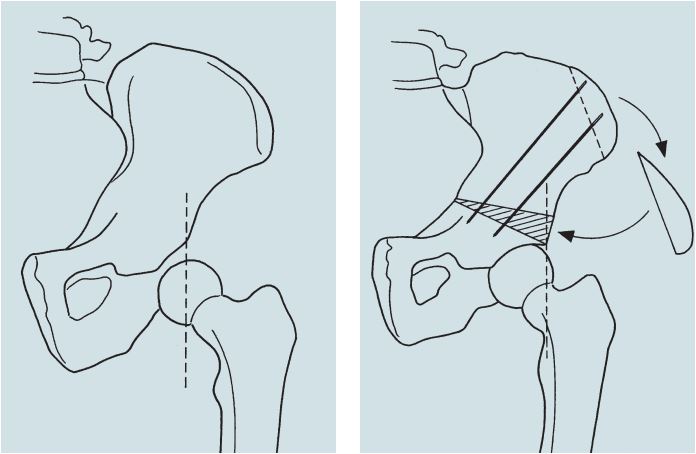
Rationale: This procedure corrects instability in the hip caused by a hip socket that is too shallow (acetabular dysplasia). The surgery improves the hip socket’s ability to cover the head of the thighbone (femur).
Description: The surgeon cuts bone away from the hip socket in the pelvis, then realigns the socket and corrects its position and/or shape. Typically, we insert new bone (bone grafts) into the section of bone that was cut. Pins or screws might provide internal support. You might need to wear a cast for external support.
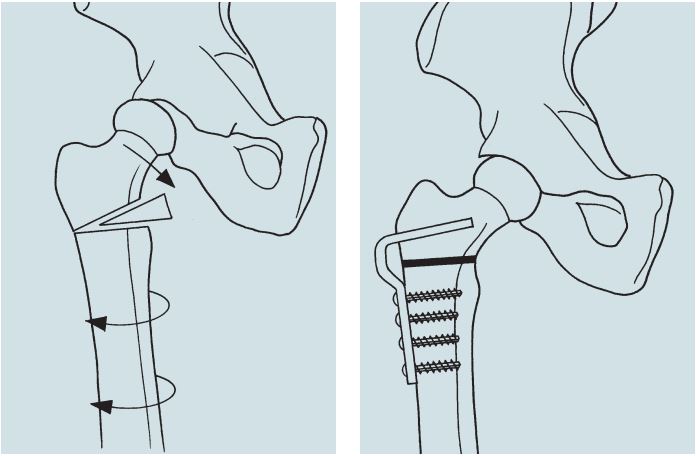
Rationale: The procedure corrects an abnormal angle or twist (excessive femoral anteversion) in the thighbone (femur), which causes the knees to rotate inward. Without treatment, bones can move out of position (hip subluxation) and intoeing can occur.
Description: The surgeon will cut the upper thighbone and correct its positioning and alignment. Metallic implants secure the cut bone.
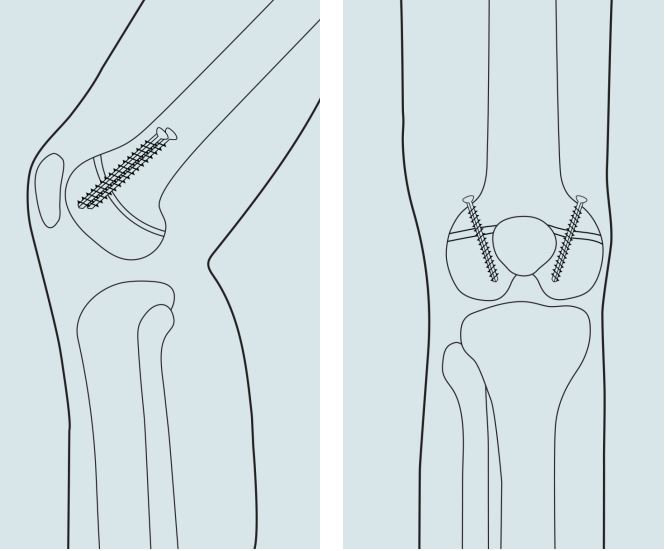
Rationale: The procedure addresses the inability to fully extend the knee (fixed knee flexion contracture). That inability might cause a crouched stance when you walk (crouch gait).
Description: The surgeon cuts the thighbone (femur) just above the knee and removes a wedge of bone to allow the knee to straighten. We then insert a metal plate and screws to maintain alignment until the bone heals.
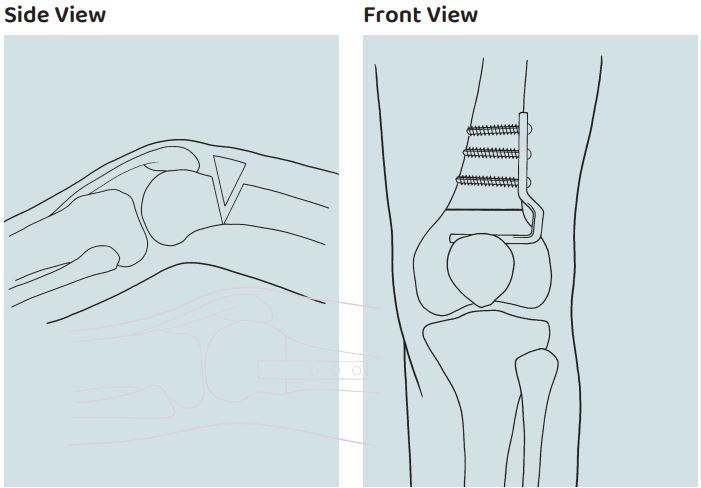
Rationale: The procedure corrects the abnormal lengthening of the kneecap (patellar) tendon, which results in a kneecap position that is higher than normal (patella alta). The abnormality can make it difficult to extend the knee fully. Walking with a crouched stance (crouch gait) might lead to knee pain and arthritis.
Description: After your bones have matured, a surgeon can move a block of bone (with the patellar tendon attached) from the upper end of the shinbone (tibia) to a lower point on the tibia. We secure the block of bone to the new position with metal screws or wires.
If your bones haven’t yet matured, a growth plate at the site of the patellar tendon attachment will prevent the surgeon from removing a bone block. In such cases, we move the tendon without removing a bone block and secure the tendon to the bone with screws and/or sutures. We use a wire or suture to attach the kneecap to the tibia, preventing the tendon advancement from pulling loose.
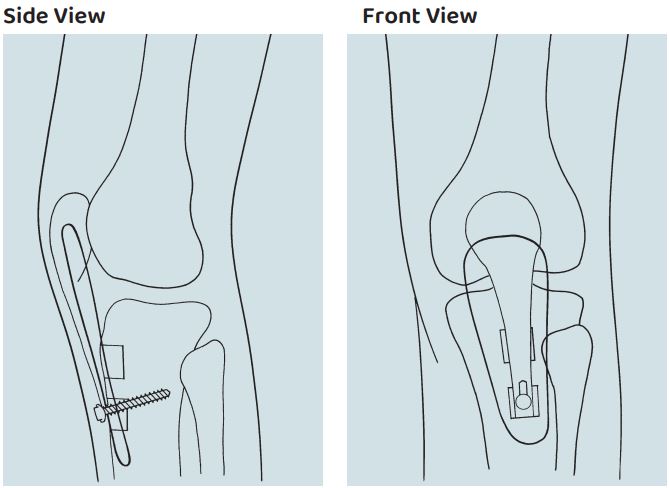
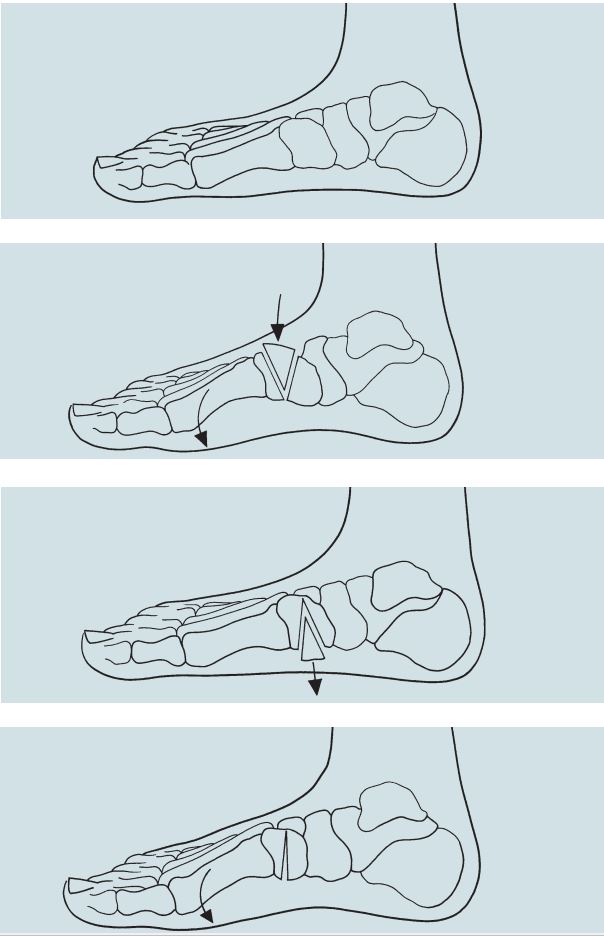
Rationale: This procedure addresses the inability to fully extend the knee (fixed knee flexion contracture). That inability might cause a crouched gait when you walk (walking with the knees bent). This surgery can treat mild to moderate contractures if there is enough growth remaining.
Description: The surgeon makes small cuts just above the knee on either side of the kneecap. A screw or a small plate + screws are inserted in each location to manipulate the front of the growth plate and slowly straighten the knee over time (months).
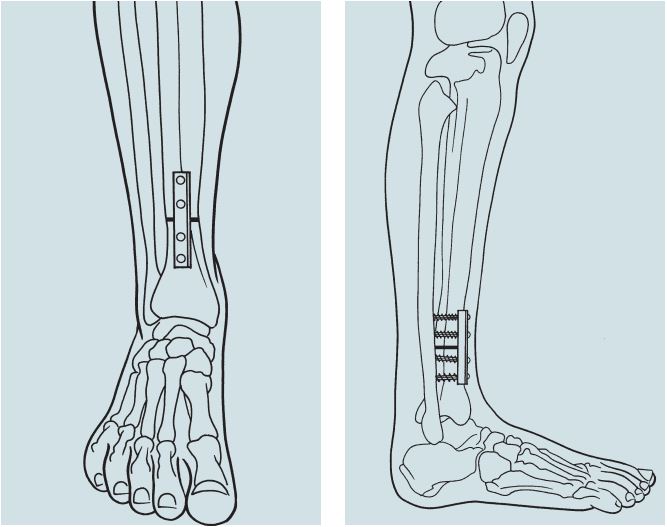
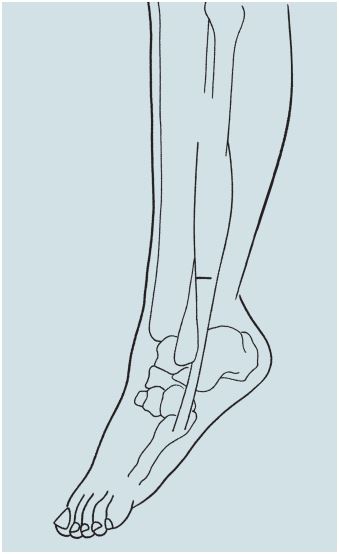
Rationale: The procedure corrects an abnormal twist or rotation in the shinbone (tibial torsion) that can lead to intoeing or outoeing. The twist prevents the foot and knee from aligning properly. In addition, it can lessen the ability of the calf muscles to maintain upright body position and push off with power when walking.
Description: The surgeon makes an incision on the front of the lower leg, just above the ankle. We cut the tibia and turn the bone to correct the abnormal rotation. Finally, we insert a metal implant to maintain proper alignment until the bone heals.
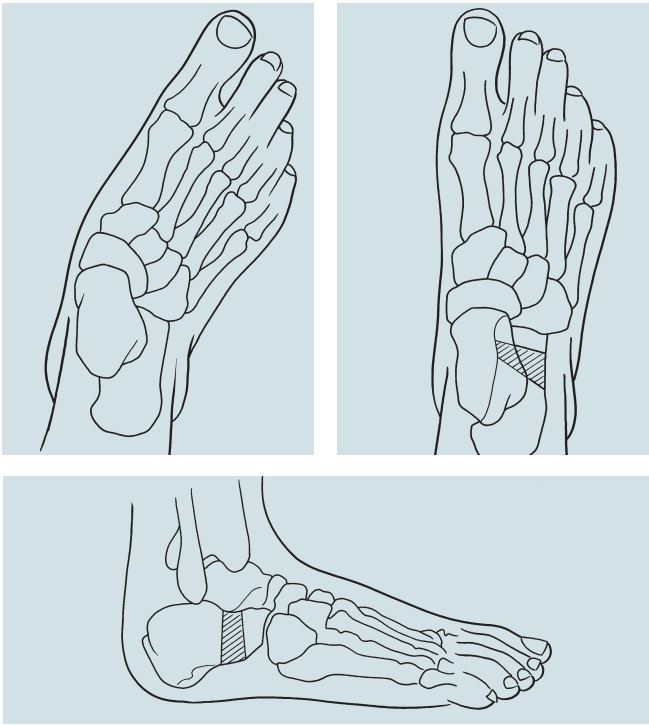
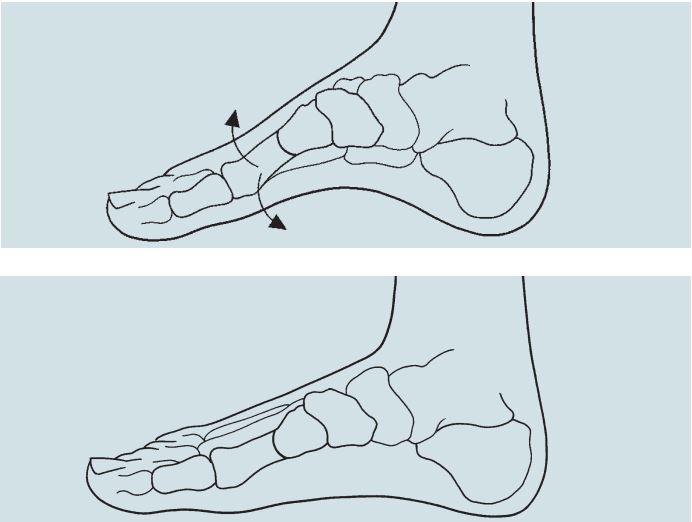
Rationale: This procedure helps correct a flat foot. A significant flat foot can affect your ability to stand upright. It can contribute to a crouched gait and reduce your ability to push off with power when walking. It often leads to outward rotation of the foot (outoeing) and can become painful.
Description: The surgeon cuts the heel bone (calcaneus) through an incision on the outer side of the foot and inserts new bone (a bone graft) to improve alignment.
Occasionally, the tendon (peroneus brevis) is too short to allow realignment of the foot with a bone graft. In that case, the surgeon might lengthen the tendon. Calcaneal lengthening can be done with other procedures, such as other calcaneal osteotomies, alonavicular fusion, first metatarsal osteotomy, or medial cuneiform osteotomy.
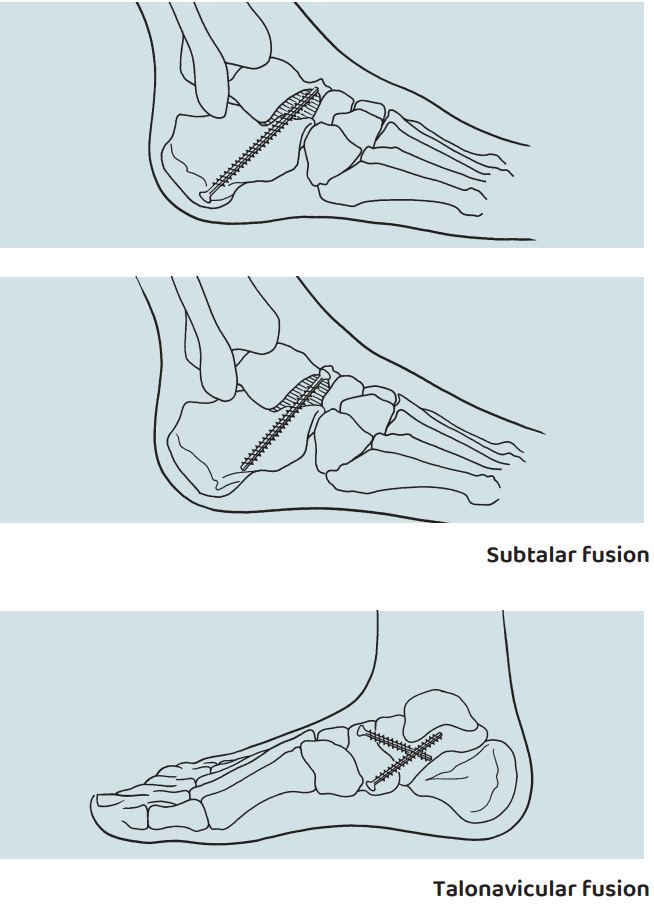
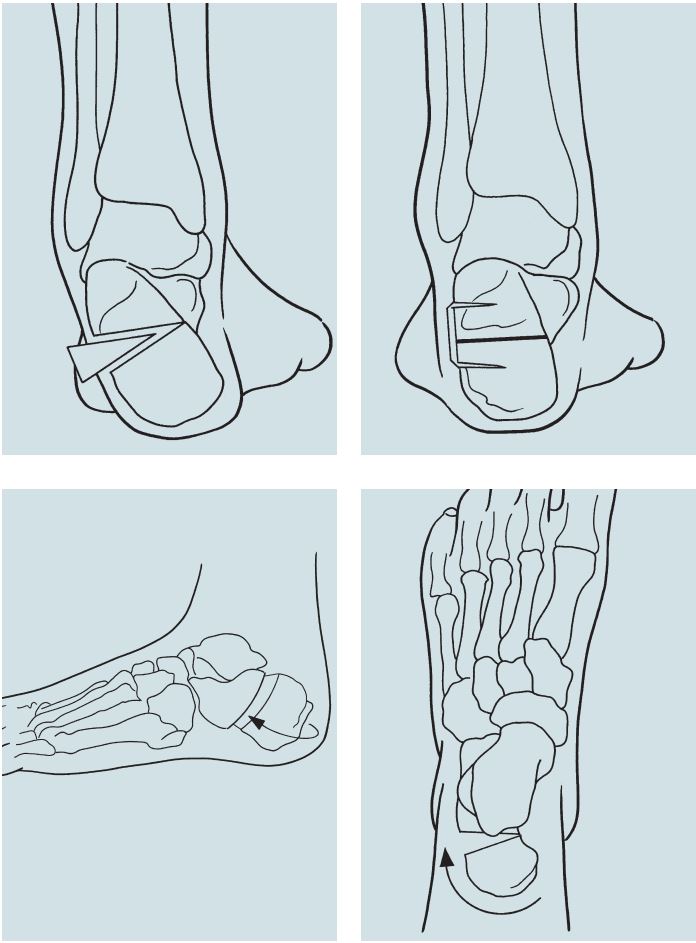
Rationale: In some cases, the muscles in the foot can’t maintain the stability of the foot’s joints. Fusing the joint might be the only way to maintain proper foot alignment and eliminate joint instability.
Description: The surgeon removes joint surfaces and fuses the ends of the bones, then inserts one or two screws to maintain alignment as the bones heal. Ankle motion (the up-and-down motion of the foot) is maintained, but the ability to roll the foot in and out decreases.
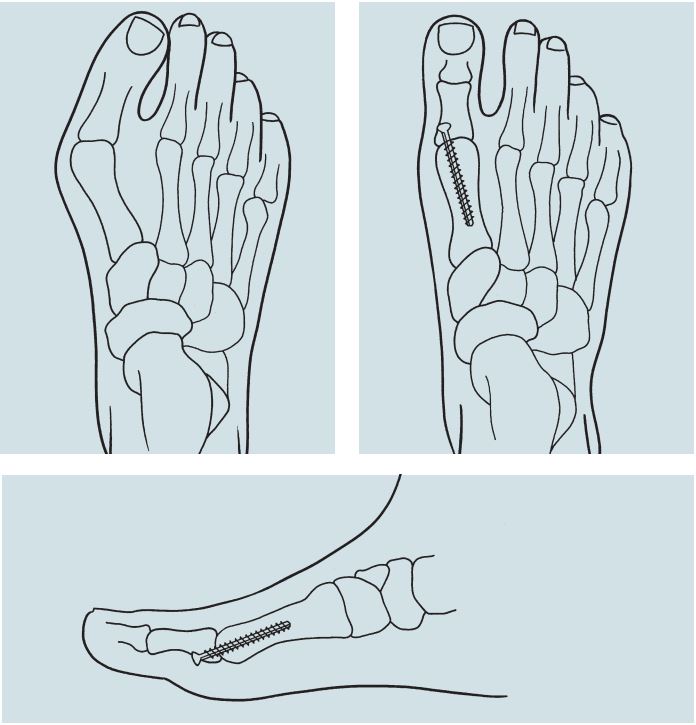
Rationale: The procedure corrects a forefoot deformity by uniformly distributing weight on the forefoot.
Description: On the inner side of the foot, the surgeon cuts and realigns the first metatarsal (bone in the arch leading to the big toe). We insert metallic implants to maintain alignment until the bone has healed.
Rationale: The procedure corrects a forefoot deformity by uniformly distributing weight on the front of the foot (forefoot).
Description: On the inner side of the foot, the surgeon cuts and realigns the bone in the arch (medial cuneiform). We might insert metallic implants to maintain alignment until the bone heals.
Rationale: The procedure corrects a bunion deformity.
Description: The surgeon removes the joint at the base of the big toe and fuses the ends of the bones. Metallic implants maintain alignment until the bone heals.
Rationale: The procedure corrects a situation in which the heel rests in a rigid position, forcing a patient to walk on the inner or outer side of the foot.
Description: The surgeon cuts the heel bone through an incision on the outer side of the heel, then repositions the bone directly beneath and in line with the shinbone. We might use metal implants to stabilize the osteotomy.
SEMLS Soft Tissue Procedures
Muscles and tendons are known as soft tissues. Soft-tissue procedures during SEMLS adjust imbalances that cause problems in the legs and feet. To prevent the reoccurrence of soft-tissue deformities corrected during a SEMLS procedure, it is recommended that issues with muscle tone are treated before surgery.
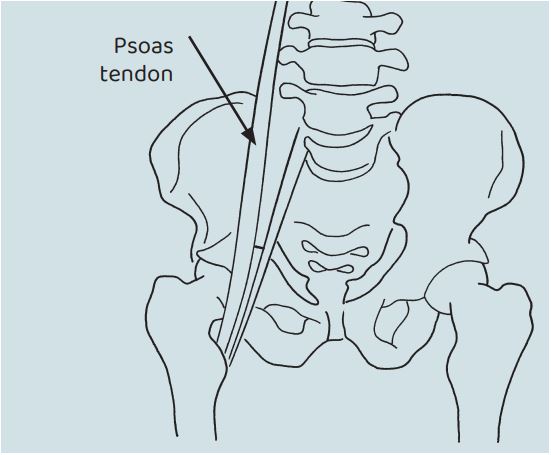
Rationale: If the psoas tendon is short or spastic, the hip can't extend fully. That can cause you to lean forward or arch your lower back.
Description: Through an incision in front of the hip joint, the surgeon divides the tendon, allowing it to lengthen while leaving muscle fibers intact.
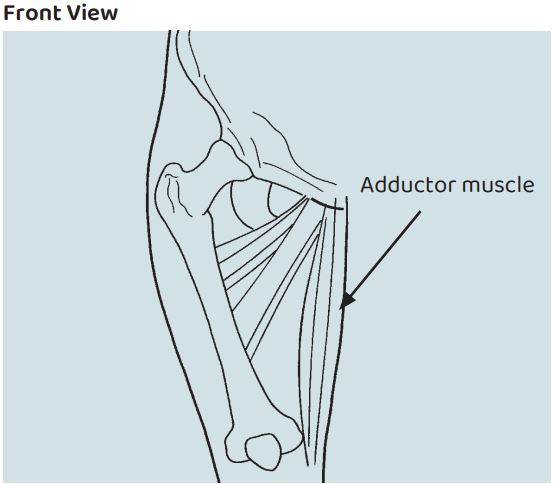
Rationale: Occasionally, the inner groin muscles restrict outward movement of the thigh (abduction). That can cause the socket to form abnormally, and it occasionally will cause a scissoring gait.
Description: Through a small incision in the groin, the surgeon divides the adductor muscles. Proper healing requires positioning and therapy.
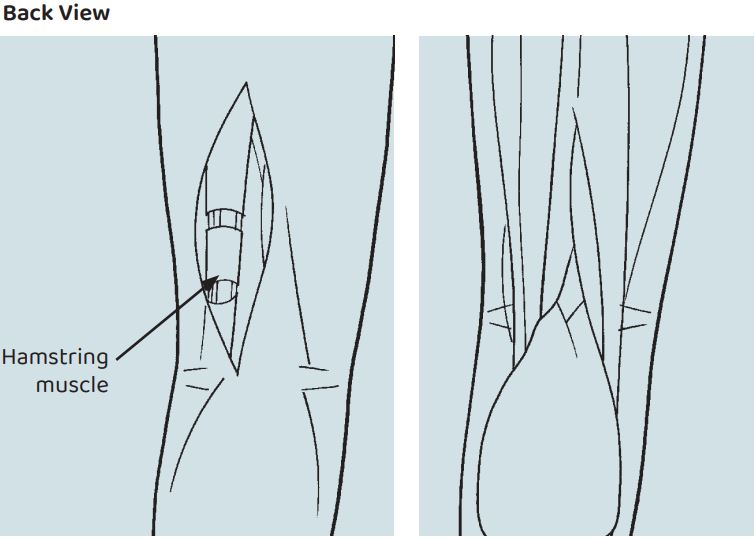
Rationale: A short or spastic hamstring can limit the ability to extend the knee. It also can disrupt the normal curve of the lower back, causing a flat back.
Description: Through an incision just above and behind the knee, the surgeon exposes the hamstring tendons and muscles. Then we use a variety of methods to lengthen the tendons.
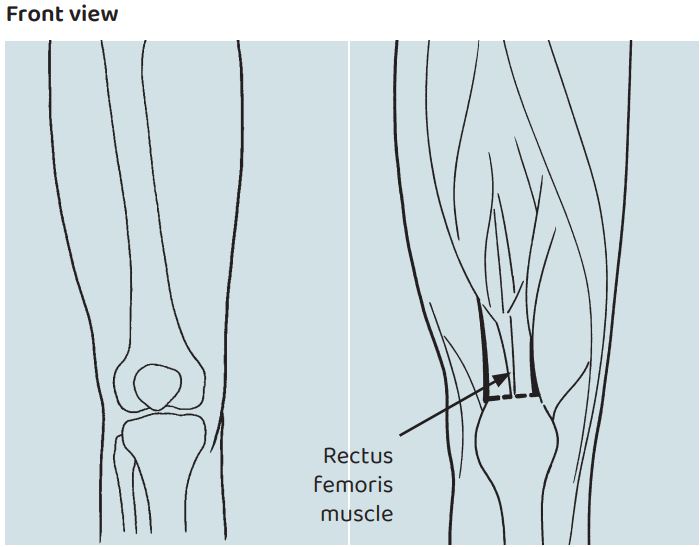
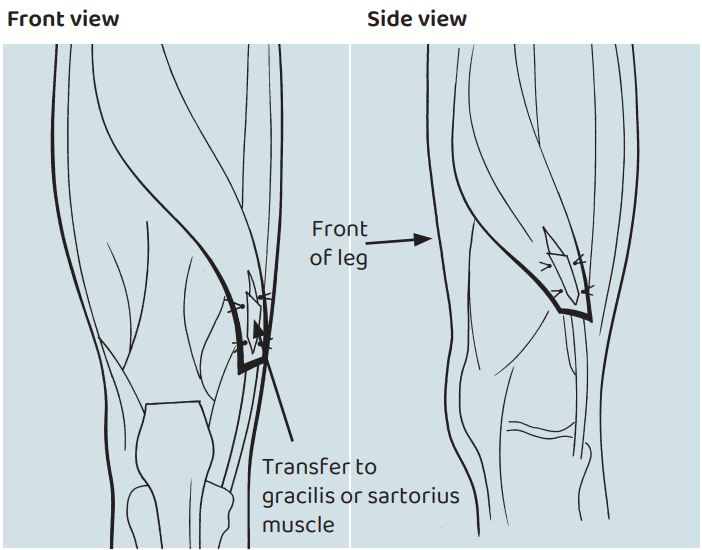
Rationale: The rectus femoris is a small, but long, muscle in the front of the thigh. When it is spastic or shortened, it can limit the ability to bend the knee and lead to a stiff gait. Transferring the muscle from its insertion on the kneecap to one of the hamstring tendons allows the knee to flex more readily.
Description: Sometimes, lengthening of the tendon can be performed without transfer. The surgeon detaches the tendon through an incision just above the kneecap. The muscle in the lower thigh can then pass closer to the inner side of the lower thigh. We typically secure the tendon to the gracilis or sartorius muscles.
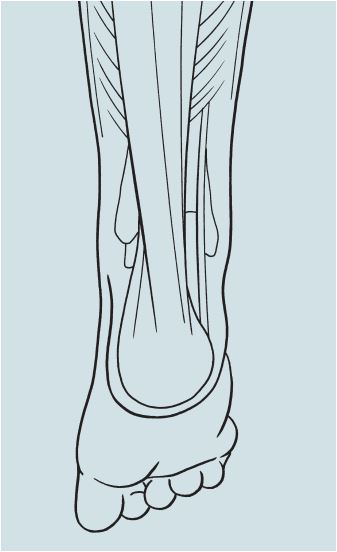
Rationale: Overactivity or shortness of the calf muscle (gastrocnemius) can lead to toe-walking, a lack of heel strike when walking, dragging of the toes, or a tendency to hyperextend the knee (back-knee).
Description: Through an incision in the middle portion of the calf, the surgeon divides the muscle from its overlying connective tissue (fascia) and tendon. We might lengthen the connective tissue surrounding the muscle on the tendon to decrease the angle between the foot and the leg (dorsiflexion) and improve movement.
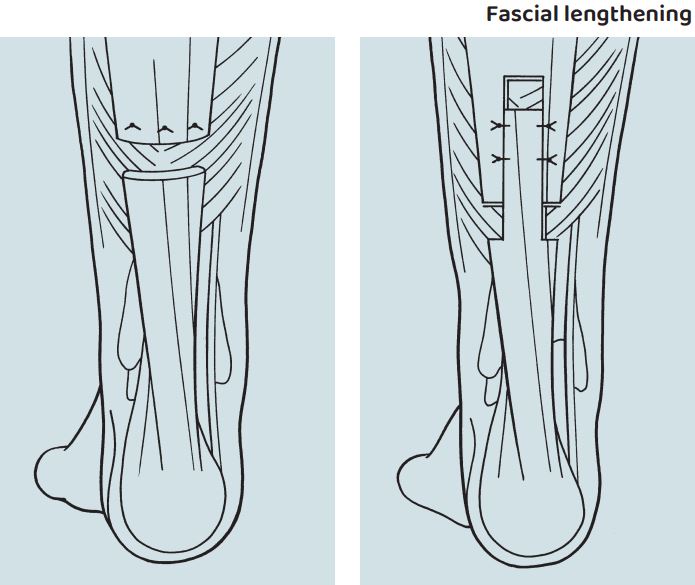
Rationale: Overactivity or shortness (contracture) of both calf muscles (gastrocnemius and soleus) can cause toe walking, severe hyperextension of the knee (back-knee), or difficulty positioning the foot in a brace.
Description: The surgeon divides the Achilles tendon in two places through one or two incisions in the lower part of the calf. The procedure enables the foot to assume a more typical position for walking or bracing. We’ll reconnect the tendon with a few sutures if needed.
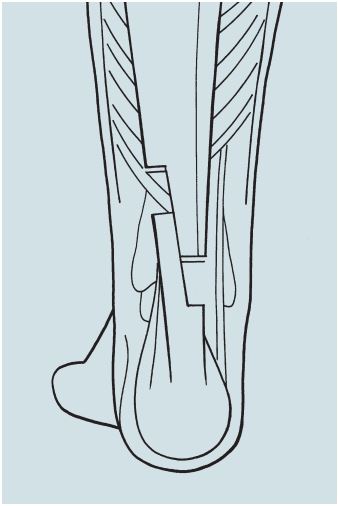
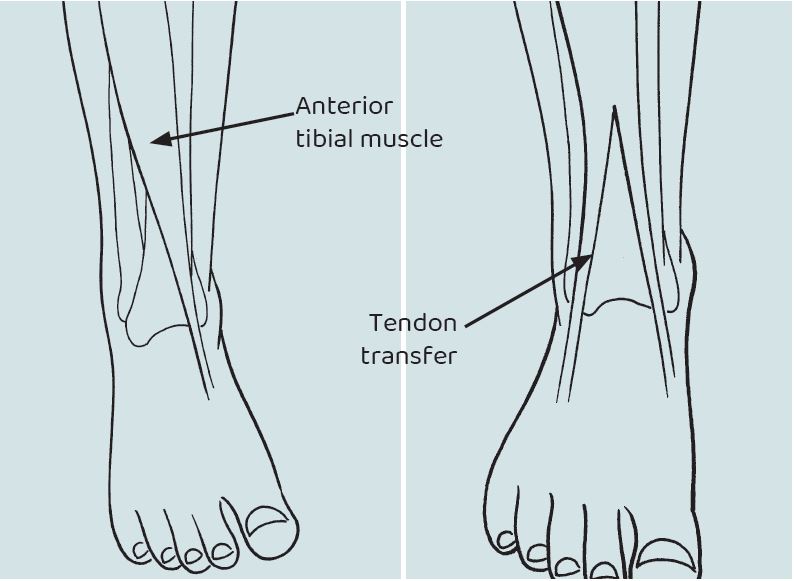
Rationale: Overactivity or shortness (contracture) of the shinbone (tibia) tendon can cause the foot to bear weight abnormally, causing inward rotation (intoeing) or high arch (cavus). Surgery balances the muscles that control motion in the back and middle of the foot (subtalar joint complex).
Description: The surgeon removes half of the tendon from its attachment to the bone. We split the tendon upward above the ankle, route the detached half to a new position, and secure it to the bone. A complete transfer involves dividing the attachment of the tendon in the foot, moving the tendon to a new bone, and resecuring it with a suture or bone anchor.
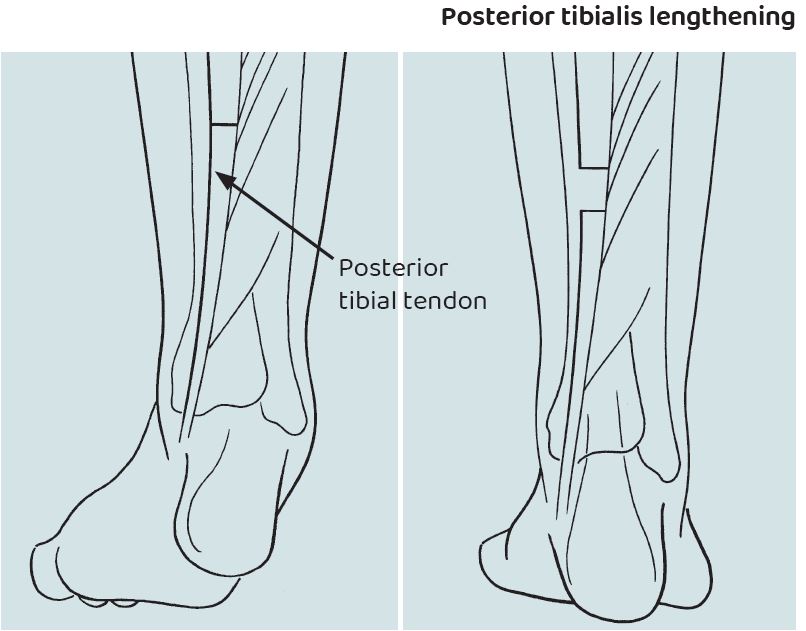
Rationale: Overactivity or shortness (contracture) of the calf tendon (posterior tibial tendon) can cause the foot to bear weight abnormally. That causes inward rotation (intoeing) or high arch (cavus). Surgery balances the muscles that control motion in the back and middle of the foot (subtalar joint complex).
Description: The surgeon might lengthen the tendon by dividing it within the muscle belly (intramuscularly) or by doing a step-cut within the tendon (z-lengthening) to gain extra length. Split transfers are more common than complete transfers. We remove half of the tendon from its attachment to the bone. We split the tendon upward above the ankle, route the detached half to a new position and resecure it to the bone. A complete transfer involves dividing the attachment of the tendon in the foot, moving the tendon to a new bone, and resecuring it with a suture or bone anchor.
Rationale: Tightness of the tendon on the outer ankle (peroneus brevis) might lead to flat feet. If the tendon is especially tight, it can limit the surgeon's ability to correct a flat foot deformity with calcaneal lengthening (see page 28). In such cases, the surgeon will lengthen the tendon.
Description: The surgeon makes an incision on the outer part of the ankle. The surgeon might lengthen the tendon by dividing the muscle belly (intramuscularly) or by doing a step-cut within the tendon (z-lengthening) to gain extra length.
 Home Page
Home Page
