How is the Gastrojejunostomy (GJ) Tube placed?
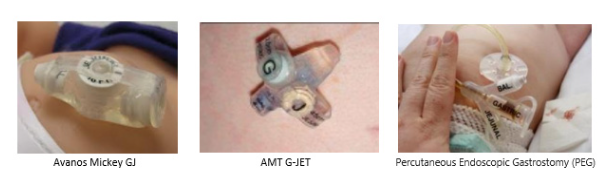
Gastrojejunostomy (GJ) tubes are typically placed using a procedure called a laparoscopy. A laparoscopy is a technique that is performed using a camera that allows a provider to see inside the child’s abdomen. The camera is placed through a small incision below the belly button. A disc or button-style GJ tube then can be positioned.
The point of a GJ tube is to vent the child’s stomach for drainage or air and provided an alternate way of eating.
Expect a 1-2 night hospital stay after surgery. The parent will practice caring for and using the GJ tube to administer feedings and medications during hospitalization. A dietician will help select the appropriate formula and the amount of formula to be given each day.
All supplies that are needed to care for the tube and administer g-tube feedings will be supplied by a durable medical equipment company (DME) or homecare supply company before you leave the hospital. You will be given the contact information for the DME company and will be able to order more supplies as needed in the future.
Each child has a different recovery, but most children resume their normal activity level within a few days. For many children, Tylenol (Acetaminophen) and/or Motrin (Ibuprofen) will provide adequate pain management in the postoperative period. Stronger medicine can be used if needed.
Wash the GJ tube site daily with soap and water starting on the day after the operation. No lotions, creams or ointments are needed. You may use a gauze dressing at the site if you wish, however, do not allow a damp dressing to remain in place; change as needed.
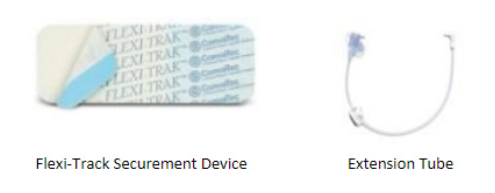
Do not rotate the tube as this can cause displacement. Keep the tube secure. If the child is on continuous feeds, use a taping device, such as a Flexi-Track, to hold the extension set in place on the abdomen.
Remove the extension set and cap the tube whenever the tube is not in use.
Your child should only have a sponge bath or shower for the first two weeks. Tub baths and swimming are okay after 2 weeks.
You will come to clinic for a post-hospital follow-up visit after the operation. Routine GJ tube changes are recommended every 4-6 months.
If you notice fever, redness or swelling at the GJ Tube site/surrounding skin, this may be sign of an infection. Call Telehealth at 651-229-3890.
What To Look For After A Gastrojejunostomy (GJ) Tube Placement
Granulation tissue: This is a common occurrence with g-tubes as healthy tissue comes out of the opening in an effort to close the hole. It appears pink/red, moist and fleshy and gives off a gold crusty drainage. This can be evaluated in clinic and treated with either silver nitrate or steroid cream. Call to schedule an appointment.

Drainage: Some drainage (yellow, gold, brown, white) from a g-tube can be seen from normal stomach secretions, this can be wiped away or dressings exchanged as needed.
Leaking: This is a common problem and often self-limited. Too much leakage means your child will not receive adequate fluid and nutrition. If you notice leakage, call Telehealth to discuss strategies to minimize leaking such as slowing the feedings down and venting the tube. If leaking occurs, protect the skin from irritation by applying zinc oxide (diaper rash cream) to the tube site, and keep the site covered with gauze.
Tube dislodgement: The g-tube can come out if the retention balloon loses water or if it is pulled out by accident. If the tube is new (less than 3 months old) and falls out and have a g-tube only available, place the tube in the hole. Never force the tube into the hole. Do not inflate the balloon. Tape the tube in place and call Telehealth who will instruct you to bring your child to the Emergency Department or Gillette clinic to have a new tube placed. Without a tube in the hole it will shrink quickly so come to the Emergency Department promptly.
GJ tube exchanges: Recommended every 4-6 months or sooner if needed. This may be done in the operating room by a surgeon or in Interventional Radiology. Please schedule as directed by the surgeon/provider. Conversion to a gastrostomy tube (stomach only) may be done in clinic.
Vomiting: If the patient begins to retch and tries to vomit, unclamp the gastrostomy tube, or access the button with the bolus exhaust tube unclamped to relieve pressure and allow the stomach contents to escape. This is called venting. If a patient has a Nissen fundoplication, it’s especially important to vent the G-tube if gagging occurs. Call your doctor if gagging or retching persists.
Illness: If the patient is sick, feedings and formula may need to be changed. Ask your doctor if the diet should be altered.
Clogging: If the tube clogs, call Telehealth Nursing for instructions. Rinsing the tube between medication dosing and feedings will usually prevent clogging.
Feeding through Gastrojejunostomy (GJ) Tube
Before feeding, check to see if the stomach is empty, if directed to do so by the patient’s doctor. Attach a syringe, allow any stomach contents to flow out via gravity by holding the syringe below the level of the stomach, and then hold the syringe up to return the contents to the stomach.
To be certain the tube remains securely positioned, gently pull back on the tube until slight resistance is felt.
If the G-tube is a button with an inflatable balloon, do not try to achieve a different fit by altering the water in the balloon. See a provider to resize.
Gravity/Bolus method
- Attach a 60ml syringe to the gastrostomy tube.
- Fill the syringe with feeding formula.
- Raise the syringe and tube 4 to 4 3/4 inches above the abdominal wall.
- Feed slowly, taking 20-30 minutes.
- Fill the syringe with the remaining fluid before it is empty, to avoid putting air into the stomach.
- DO NOT give gravity/bolus feedings through the jejunostomy tube.
Pump method
- Fill the feeding bag with the desired amount of fluid.
- Drain fluid to the end of the tube to remove the excess air in the tubing.
- Connect the tubing to the gastrostomy or the jejunostomy port as directed.
- Usually, jejunostomy feedings are all done with feeding pump over several hours
- Begin the pump at the rate of _____ ml per hour.
- Make sure your child is as safe as possible during feeding. You can prevent accidental choking by placing the tubing out of your child’s reach and away from their head, neck, and shoulder area while they are connected to the feeding bag.
- Place the patient in a comfortable position either upright or at an incline. Infants should be placed in an infant seat or held.
- It is best not to feed the patient when they are lying flat. If necessary, place them on their right side.
- Put _____ ml of water in the feeding bag or syringe and repeat the same feeding procedure to clean the tubing.
- Disconnect the syringe or the tubing and plug the end of the gastrostomy tube.
- The patient should sit up for 30 minutes after each feeding.
How should medicine be administered?
- Medicines given by gastrostomy should be in liquid form or, if approved by your doctor, finely crushed and dissolved in liquid. Try to avoid medicines in sprinkle form. These may clog the G-tube.
- Give medicines by the gravity method using a syringe. If it is a button style G-tube, use the bolus extension tube to give crushed medicine. Do not use the right angle tube for this.
- Flush with 10-30 ml of water after giving medicines. Your doctor or nurse will tell you how much water to use based on the patient’s size and need for fluids.
Your Care Team
Our providers are here for you every step of the way, so never hesitate to call us.
Gillette Pediatric Surgery Team Contact Information:Telehealth 651-229-3890
- Midwest Radiology 651-917-9330
- U of M Interventional Radiology Scheduling 612-273-6378
- Children’s Interventional Radiology Scheduling 612-874-5399
Translations
This information is for educational purposes only. It is not intended to replace the advice of your health care providers. If you have any questions, talk with your doctor or others on your health care team.
If you are a Gillette patient with urgent questions or concerns, please contact Telehealth Nursing at 651-229-3890.
 Home Page
Home Page
