Maggie Anderson's journey with Physical Therapy Scoliosis-Specific Exercises (PSSE) began during a routine physical in 2019. Her pediatrician suggested she get a scoliosis evaluation at Gillette because she saw a slight curve in Maggie’s spine. After imaging, X-rays revealed she had four curves in her spine.
“When I first saw that X-ray of my spine I was flabbergasted. To me, my spine looked really messed up,“ Maggie recalls.
At the time, Maggie played volleyball in school and was very committed to athletics. She and her mother were concerned her scoliosis diagnosis would have an impact on Maggie’s athletic activity. Maggie was determined to do everything she needed to do to keep active, so she jumped at the chance to work with the Gillette physical therapy experts to strengthen her muscles and improve her chances of stopping her spinal curve from progressing.
What Is PSSE?
PSSE is a conservative treatment for scoliosis. It uses exercises customized to each person to reduce the symptoms of scoliosis. Two Gillette physical therapists, Michelle Engberg and Katie Wilkins, have undergone extensive training to become experts in PSSE.
“One of the benefits of getting PSSE and working with a physical therapist is that we can help improve the flexibility of the spines that are stiff,“ Michelle Engberg, PT, says. “This can help with posture and make bracing easier. For spines that are already flexible, PSSE can strengthen and teach stabilization in the best position possible for that spine.“
Experts from the Gillette Spine Institute can determine if PSSE is an appropriate treatment for patients who are 10 years of age and older, have adolescent idiopathic scoliosis, and have a spinal curve approximately 20 degrees or greater.
“The goal of our exercises is to de-rotate, elongate, and stabilize the spine in a three-dimensional plane,“ Katie Wilkins, PT, says. “Every exercise we do with a patient is aimed at setting them up for best positioning. This PSSE therapy can help with things like an elevated shoulder, a trunk that is slightly shifted, or issues with the hip,“ Wilkins adds.
Maggie and her mother appreciate the care from the Gillette physical therapy team and the Spine Institute. She credits the great support and care she receives from Enberg and Wilkins as one of the main factors in her embracing scoliosis and seeing it as part of her journey in life.
“Michelle and Katie knew how to support me when I was at my most vulnerable,“ Maggie says. “They answered all my questions, and it became a relationship beyond physical therapy.“
How and When to Refer to Scoliosis Experts
With a highly collaborative team and support from the organization, Gillette Children's Spine Institute can offer services that expertly manage routine care as well as rare and complex spine conditions and injuries.
- Back Pain
- Bulging Disc
- Coccyx/Tail Bone Pain
- Disc Degeneration
- Disc Herniation (slipped Disc)
- Kyphosis
- Lordosis with XRs
- Neck Pain (Cervical Spine Issues)
- Revision Spinal Fusion
- Scheuermann's Disease
- Scoliosis (Congenital, Idiopathic, Neuromuscular)
- Spine Fractures/Spine Trauma
- Spine issues related to Skeletal Dysplasia
- Spine issues related to Spina Bifida
- Spine issues related to Spinal Cord Injury
- Spine Tumor
- Spondylolysis/Spondylolisthesis
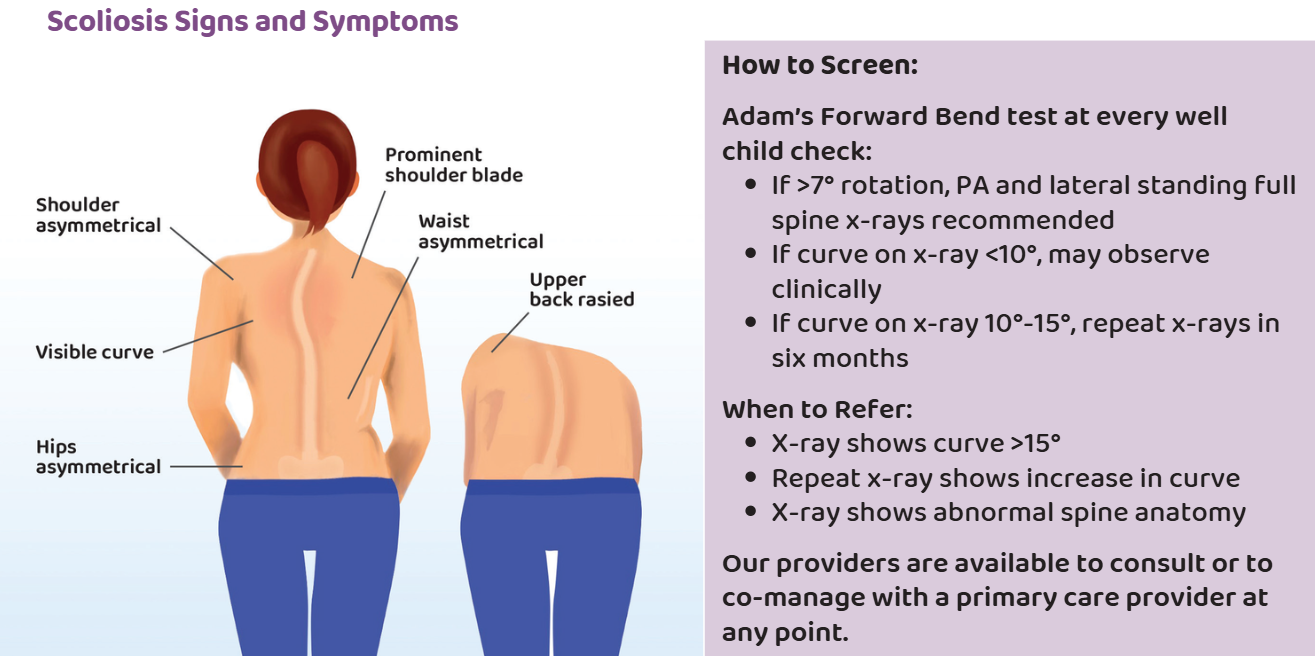
Identifying Scoliosis
Scoliosis is one of the most common pediatric spine conditions you may encounter in your day-to-day practice. When you suspect your patient may need a pediatric spine specialist for their scoliosis, there are some easy signs and symptoms you can look for.
Understanding Scoliosis Treatments
The degree of curvature and skeletal maturity of the patient are important considerations when recommending treatment for scoliosis symptoms.
| Degree of Curve | Course of Action |
|---|---|
| <10 degrees | Observe clinically over time |
| 10-20 degrees | Periodic X-rays |
| 20-45 degrees | TLSO or Nighttime bracing |
| >45 degrees | Surgical intervention; fusions at any skeletal maturity |
| Any curvature | SCHROTH (scoliosis-specific exercise) |
| Further evaluations needed to qualify | VBT (vertebral body tethering); skeletally immature |
Join Our Partners in Care Community!
Subscribe to Partners in Care Journal, a newsletter for medical professionals.
Subscribe Today Home Page
Home Page

