What Is Invasive EEG Monitoring?
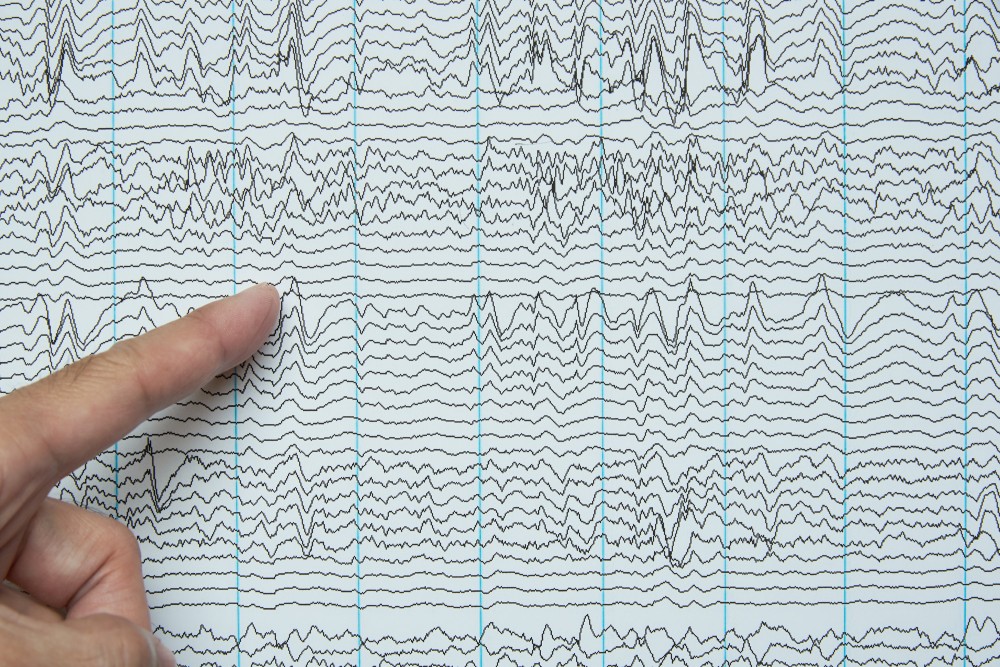
Invasive EEG monitoring is a type of electroencephalography (EEG) that is recorded intracranially, or directly from the brain. Intracranial EEG is the gold standard for localizing where in the brain seizures start (epileptogenic zone), as it is more specific than a noninvasive (scalp) EEG test. For invasive EEG, a neurosurgeon places the recording electrodes during an operation. Electrode placement occurs under general anesthesia through a hole in the skull or a craniotomy. The location of recording will be determined by previous EEG studies, MRI, and other imaging such as Positron Emission Tomography (PET) or Single-Photon Emission Computerized Tomography (SPECT).
There are two methods of invasive EEG monitoring:
Subdural Grids and Strips: Subdural grids and strips are used when larger areas of the brain need to be covered during invasive monitoring. The electrode grids and strips are made up of small disc electrodes that are embedded in soft rubber called silastic. Configurations and the number of electrodes required vary from case to case and can range from as few as 8 electrodes up to 64 electrodes.
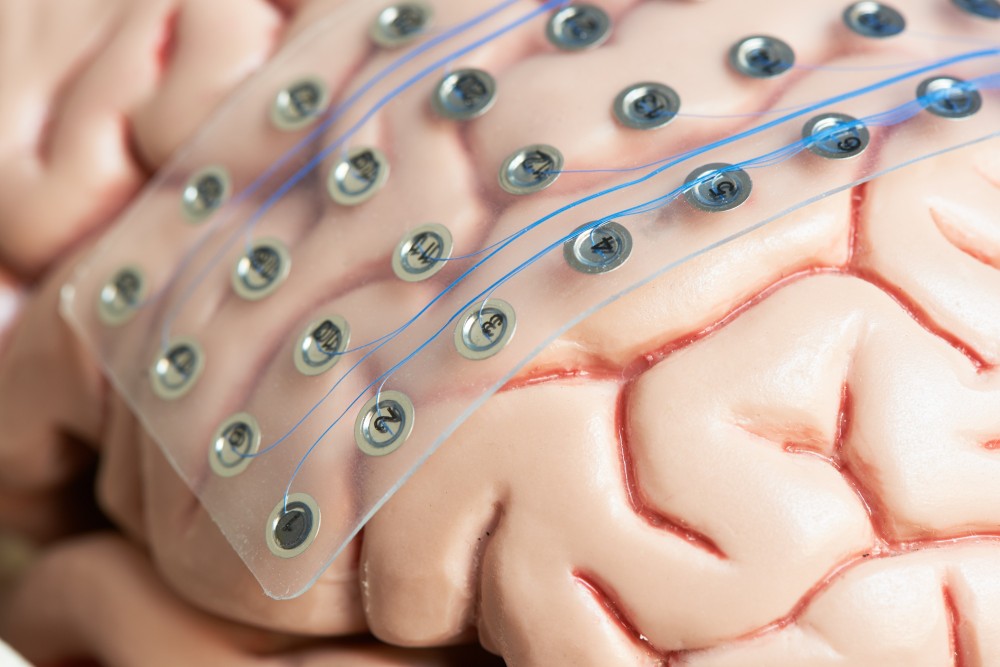
Because of their larger recording area, a craniotomy is required to place subdural grid electrodes. Grids are often used in conjunction with strip electrodes, which are arranged linearly and are best for recording from under the temporal or frontal lobes. These strips can be placed via a hole in the skull or during the same craniotomy as the grid electrode.
Stereotactic EEG (sEEG): A stereoelectroencephalography, or sEEG procedure, is thought of as less invasive than subdural grids and strips, requiring only small incisions in the scalp and skull for electrode placement. sEEG electrodes are made up of thin, flexible plastic with embedded electrodes that can record from deep parts of the brain. The electrodes are placed stereotactically, meaning the electrode placement is guided by three-dimensional imaging of your brain. Because of this minimally invasive approach, electrodes can be implanted in both hemispheres of the brain.
Who Is A Candidate For EEG Monitoring?
Invasive EEG monitoring is part of the evaluation for epilepsy surgery. By measuring the electrical activity in the brain, it helps your provider get a better understanding of a diagnosis.
Invasive EEG monitoring is generally reserved for patients with epilepsy who have not responded to medication or treatment, and whose early evaluation does not give a clear enough picture to perform a surgical intervention. Invasive monitoring may also be necessary when there is a need to define brain function near the epilepsy surgery areas.
What Can I Expect During invasive EEG monitoring?
Once the electrodes are placed in the operating room, you will have a CT scan to ensure proper placement on the brain. Then you will be taken back to your hospital room to begin EEG monitoring. The goal of invasive EEG monitoring is to record your typical seizures to better determine the epileptogenic zone. To increase the likelihood of seizures, your seizure medications may be adjusted or reduced during this time. The duration of monitoring is dependent on the frequency of your seizures.
If the epileptogenic zone is found to be close to the areas of the brain related to speech, motor and sensory function, or vision, you may have functional mapping completed during your invasive EEG monitoring. This will provide the neurosurgeon with a map of areas to avoid during any future brain surgery.
After your invasive EEG monitoring is completed, you will return to the operating room for the electrodes to be removed. Before you are discharged from the hospital, you will return to your usual seizure medication dosage and schedule.
What Are The Benefits Of Invasive EEG Monitoring?
As invasive EEG monitors directly from the brain, this allows for the detection of seizures earlier and more often than scalp electrodes. More abnormalities can be detected between seizures (interictally) as well. If you are a candidate for invasive EEG monitoring, this enables the neurology and neurosurgery team to create a surgical plan that will be safe and effective in controlling your seizure activity.
What Are The Risks Of Invasive EEG Monitoring?
The risks of invasive EEG monitoring are similar to other neurosurgeries, and may include:
- Infection
- Hemorrhage
- Cerebral edema
Next Steps
The additional EEG data gathered during your stay will be presented at the Epilepsy Patient Management Conference (PMC), where epileptologists and other epilepsy health care providers will discuss the best path forward for seizure control.
For some, surgery may be an option. To be evaluated for epilepsy surgery, you might need the following tests or consults:
- Brain imaging
- Neuropsychological evaluation
- Psychological evaluation
- Physical medicine and rehabilitation consultation
- Neurosurgery
- Invasive EEG Monitoring
- Lobectomy
Your provider can answer all of your questions and is there to talk through all of the possibilities.
Integrated Care
If your child experiences seizures or has epilepsy, we offer complete diagnostic services and a team of experts to provide comprehensive care, beginning with a first seizure evaluation by experts in nursing and neurology (pediatric neurologists, epileptologists, and neurology nurse practitioners).
As your child grows into their teen years and adulthood, we’ll continue to work closely with your family to provide the most effective management and best care for epilepsy and seizures. Over the course of treatment, your child might receive care from providers in the following specialties and services:
- Chaplaincy
- Child life
- Endocrinology
- Medical genetics and genetic counseling
- Neurodevelopmental pediatrics
- Neurodiagnostics for tests such as EEGs, VEEGs and overnight sleep studies
- Neuropsychology
- Neurosurgery
- Nutrition and feeding
- Pediatrics and general medicine
- Psychology
- Radiology and imaging
- Rehabilitation medicine
- Rehabilitation therapies, including occupational, physical, and speech and language therapy
- Sleep medicine
- Social work
- Therapeutic recreation
You can trust your child’s care to our expertise in treatment of epilepsy and seizures. As a regional leader in pediatric neurology and neurosurgery, we understand that many kids who have epilepsy also have complex associated conditions, such as cerebral palsy, developmental delays or traumatic brain injuries. That’s why we offer a large team of specialists and extensive support services.
For more information, learn about epilepsy and find resources from advocacy and support organizations like the Epilepsy Foundation.
Explore Invasive EEG Resources
This information is for educational purposes only. It is not intended to replace the advice of your health care providers. If you have any questions, talk with your doctor or others on your health care team.
If you are a Gillette patient with urgent questions or concerns, please contact Telehealth Nursing at 651-229-3890.
 Home Page
Home Page
