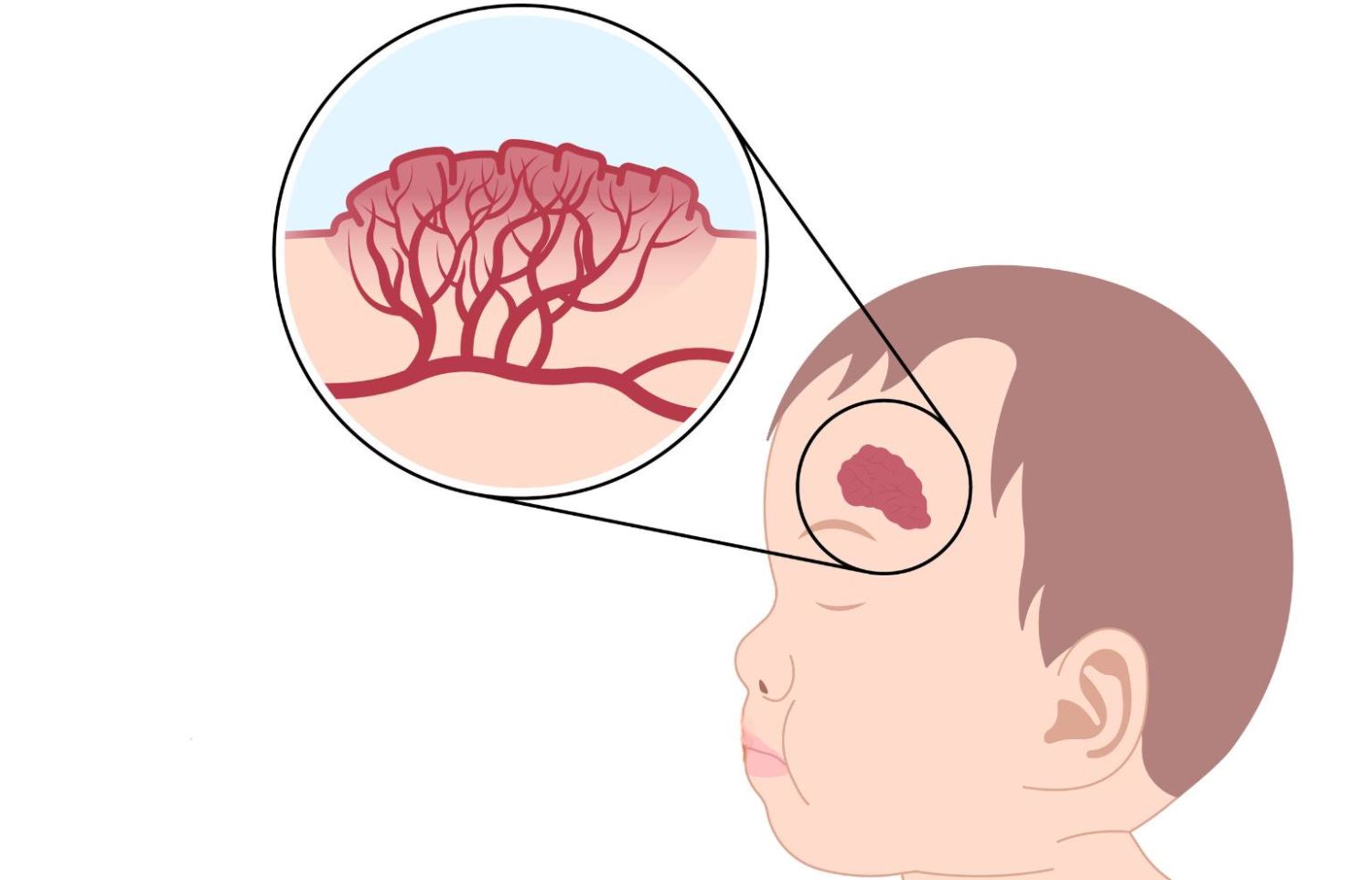
Infantile hemangioma is one of the most common benign vascular tumors, occurring in 4-5% of infants. It is characterized by a hyperpigmented, often raised area of the skin. More frequently seen in girls than in boys, it is also more common in pre-term infants, multiples (such as twins), and those with low birth weight. Infantile hemangioma is more likely to occur in white children than in those of other races.
Gillette Children's favors a multidisciplinary approach to treatment to ensure the best possible outcome for each patient. Our experienced, board-certified craniofacial and plastic surgery experts prefer to see patients with infantile hemangioma as early as possible, to determine whether treatment is necessary. If treatment is recommended, it is better to start sooner rather than later. To refer a patient to a Gillette specialist for infantile hemangioma care, call (651) 325-2200.
What are the phases of infantile hemangioma?
The onset of infantile hemangioma occurs by the time a child is four weeks of age. The proliferation phase, when the hemangioma may continue to grow and darken, occurs when a child is between one and three months old. Hemangiomas typically reach a plateau when the infant reaches five months of age. Involution, the final phase of the infantile hemangioma lifecycle, wherein it may shrink or lighten on its own, occurs by about five years of age.
What causes infantile hemangioma?
While the origin of infantile hemangioma has yet to be fully determined, experts believe it may result from a hypoxic injury (lack of sufficient oxygen to the affected tissue). In this theory of the formation of infantile hemangioma, endothelial progenitor cells migrate to locations favorable for growth and form vasculature during the proliferation phase in an attempt to normalize the hypoxic tissue.
When is infantile hemangioma considered a risk?
Six categories of infantile hemangioma are considered high-risk.
The most life-threatening infantile hemangiomas occur in the beard area of the head and neck. The primary concern with a hemangioma in this area is the potential impact on the child's airway, particularly if the hemangioma is growing inward instead of outward. Another possibly life-threatening condition is the presence of five or more cutaneous hemangiomas, which can suggest internal organ involvement such as the liver.
Another potentially high-risk hemangioma is one that causes functional impairment. For example, a hemangioma in the ocular area could cause visual disturbances, while an oral hemangioma may affect feeding.
Some infantile hemangiomas are more likely to result in ulceration or bleeding, putting them in the "high-risk" category. Another category of high-risk hemangioma is associated with a syndrome such as PHACES: Posterior fossa, Hemangioma (large plaque), Arterial anomalies, Cardiac anomalies, Eye, Sternal cleft; or LUMBAR: Lower body hemangioma and other cutaneous defects, Urogenital anomalies, Myelopathy, Bone deformities, Anorectal malformations, Arterial anomalies, Renal anomalies.
Lastly, infantile hemangioma is high-risk if it causes disfigurement in areas such as the nose or lip or if it is greater than two centimeters in size on the face or scalp.
How is infantile hemangioma diagnosed and treated?
Diagnosis of infantile hemangioma requires visual assessment. In rare cases, such as the presence of five or more cutaneous lesions, an abdominal ultrasound or MRI/MRA may be necessary. Imaging should also be considered in the presence of PHACES or LUMBAR syndromes or if the diagnosis is uncertain.
While most infantile hemangiomas are not high-risk and therefore do not require treatment, both pharmacological and non-pharmacological options exist to treat high-risk hemangioma.
Pharmacological Options
Three pharmacological options indicated for the treatment of infantile hemangioma are timolol (topical), propranolol (oral), and triamcinolone (injectable). Side effects of these medications may vary; it is best to see a board-certified pediatric craniofacial and plastic surgeon for a complete expert evaluation and recommendation.
Non-Pharmacological Options
Non-pharmacological treatment options for infantile hemangioma include lasers and excision. Laser treatment is often indicated for ulcerated or bleeding hemangiomas, although propranolol is shown to be just as effective in those cases. Laser treatment is typically prescribed following the involution phase of the hemangioma if the hyperpigmentation is bothersome to the patient or family. Excision is also indicated for the post-involution phase of the hemangioma lifecycle (in case the hemangioma resolves without surgical intervention). Holding off on excision also minimizes scarring and is generally considered safer.